Mako Robotic-Arm Assisted Total Knee Arthroplasty
Abstract
Total knee arthroplasty (TKA) has been around for decades and serves as a very successful procedure to alleviate pain and restore function in a knee with advanced degenerative joint disease. Over the years, there have been many advancements in surgical technique and even more so in implant design. One of the more recent technological breakthroughs in TKA is the use of a robotic-assisted arm for enhanced preoperative planning and intraoperative guidance with dynamic joint balancing and bone preparation. This video article outlines the operative technique used by the primary author in performing a posterior stabilizing TKA in a varus deformity degenerative knee using Mako robotic assistance.
Case Overview
Background
Knee osteoarthritis is a degenerative disease that causes progressive loss of articular cartilage. The incidence of symptomatic knee osteoarthritis is around 240 per 100,000 per year. Risk factors include articular trauma, an occupation requiring repetitive knee bending, muscle weakness, large body mass, female gender, increased age, genetics, race (White > Hispanic > African American), and metabolic syndrome (a syndrome consisting of central or abdominal obesity, dyslipidemia, high blood pressure, and elevated fasting glucose levels). Pathophysiologic changes to the articular cartilage include increased water content, the collagen becomes disorganized, proteoglycans become altered and eventually decrease in amount, but the chondrocyte size and number stay the same. The subchondral bone attempts to remodel, forming lytic cysts with surrounding sclerosis. Bony osteophytes also form through pathologic activation of endochondral ossification. The synovium goes through progressive inflammatory changes, eventually becoming hypervascular and increasingly thick.
Focused History of the Patient
The patient is a 66-year-old female who presents with a 2-year history of left knee pain without history of injury or trauma. The pain is exacerbated by prolonged ambulation, climbing stairs, and prolonged standing. Treatments tried have included bracing, anti-inflammatory oral medications, corticosteroid injections with good temporary relief, and formal physical therapy. She has a past medical history of hypertension, hyperlipidemia, and anxiety.
Physical Exam
The patient was comfortable, well-appearing, and oriented to time, place, and person. She ambulated with an antalgic gait. Examination of her left lower extremity revealed the skin was clean and intact throughout. Thigh and leg compartments were soft. She had a normal hip range of motion without pain. Grossly, her knee was in mild varus deformity. There was a moderate knee effusion. She had a knee range of motion from 0° to 115° of flexion. She had tenderness over the medial joint line. Her knee ligament exam was stable to the anterior drawer, Lachman, posterior drawer, and the varus and valgus stress testing. Her extensor mechanism was intact, and she had no pain with straight leg raise. She was neurovascularly intact distally.
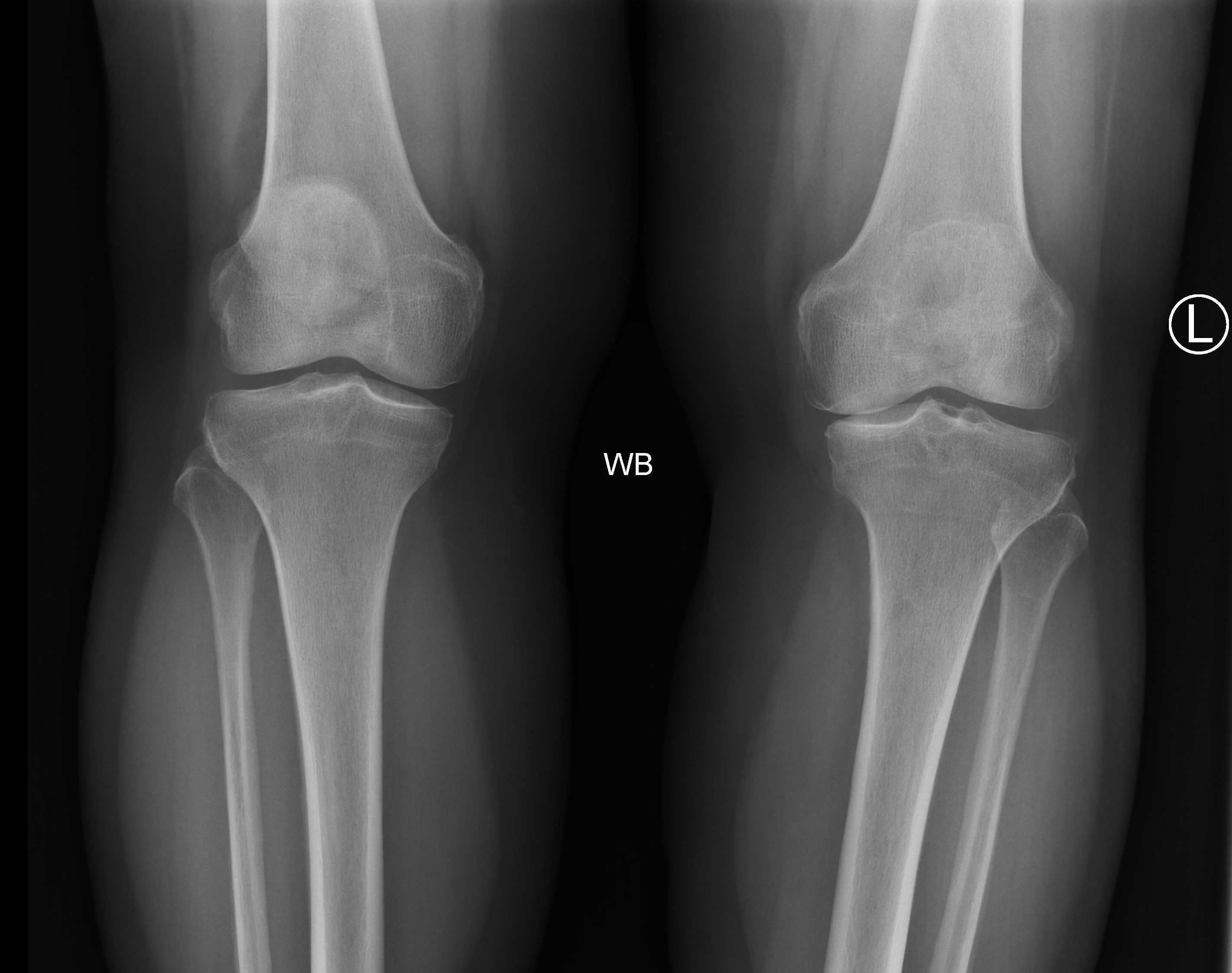
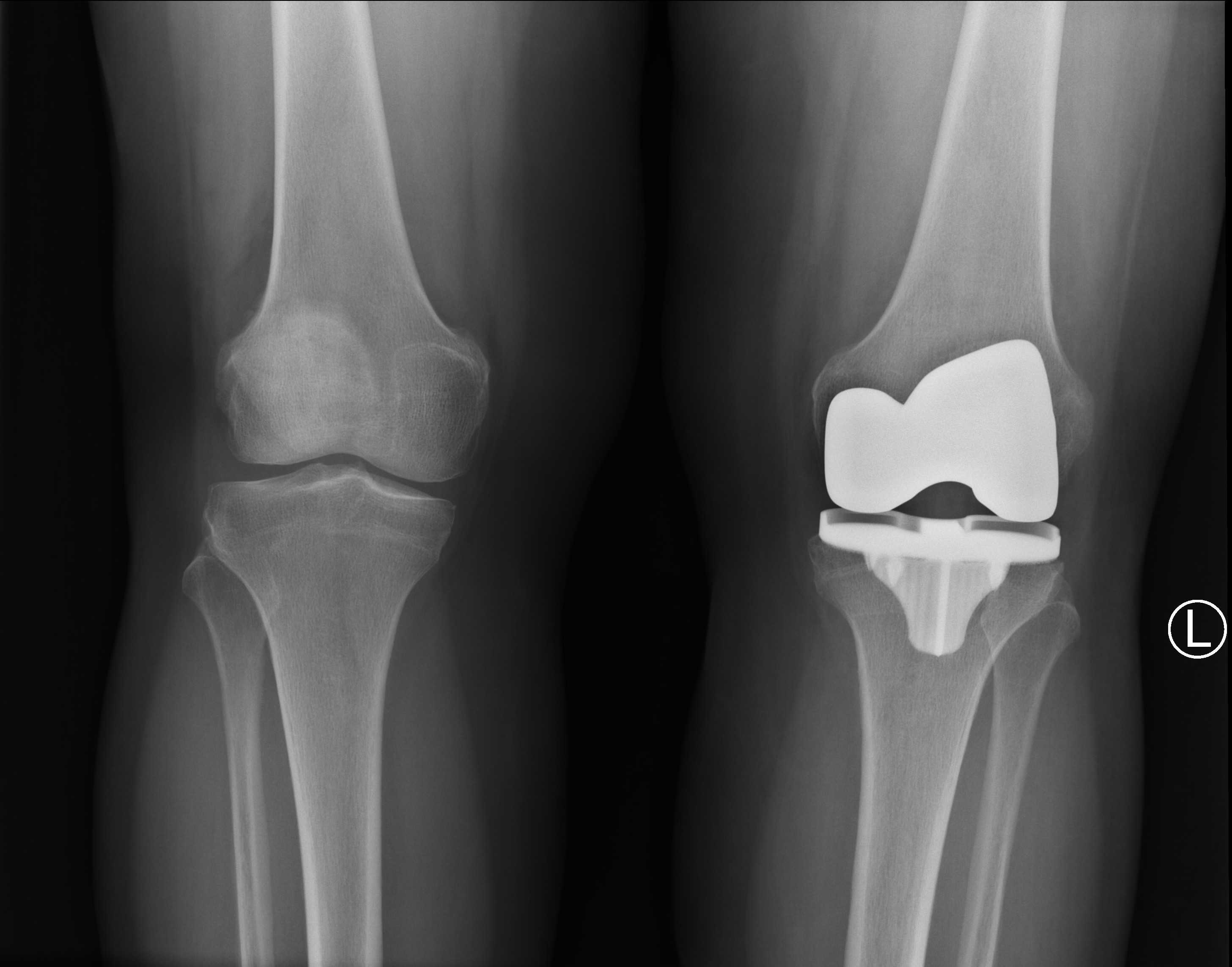
Imaging Studies
Important radiographs to take before deciding to proceed with a total knee arthroplasty (TKA) include weight-bearing AP, PA flexion, lateral, and sunrise views. Some surgeons also like to review long leg alignment radiographs. The images for this patient revealed severe degenerative changes with loss of joint space in the medial and patellofemoral compartment with bone-on-bone contact, subchondral sclerosis, and multiple periarticular osteophytes. There was mild varus mechanical alignment. The patella was tracking centrally on the sunrise view.
Additionally, a CT scan was obtained per the Mako protocol in order to perform preoperative planning and allow the Mako robot to perform accurate intraoperative guidance. The CT protocol is provided by Mako.
Natural History
The natural history of osteoarthritis is progressive, leading to increasing pain and disability. However, the rate of symptomatic progression is variable from patient to patient. In general, it is a slow progression where symptoms become more severe, frequent, and debilitating over months to years. As the arthritis and deformity worsen over time, patients experience a decline in their function including range of motion and ability to ambulate. Some patients have severe symptoms with only mild disease visualized on radiographs while others have little to no symptoms with severe radiographic disease. Surgeons should treat the patient and his or her symptoms.
Options for Treatment
Treatment for osteoarthritic knees typically begins with non-operative management including activity modification such as reducing impact loading exercises and reducing weight. Nonsteroidal anti-inflammatory drugs (NSAIDs) are also first-line treatment. Other non-operative treatment options include acetaminophen, physical therapy, corticosteroid injections, bracing, and the use of an assistive device such as a cane or crutch. A surgical option that is typically reserved for younger patients with isolated medial or lateral compartment arthritis is an osteotomy to off-load the affected compartment and correct deformity. Joint replacement options include partial knee replacement and total knee replacement. Risks and benefits to arthroplasty are weighed on an individual basis. Risks include, but are not limited to, infection, bleeding, blood clots, damage to surrounding structures, wound healing issues, leg length discrepancy, instability, continued pain, stiffness, fracture, and need for further surgery.
Rationale for Treatment
TKA is a successful surgical procedure that reliably provides pain relief and improved function in patients with degenerative joint disease. The patient presented with degenerative changes of the left knee. She had severe pain associated with activity and radiographic findings of moderate to severe arthritis. She had failed to obtain adequate function or pain relief with walking aids, bracing, physical therapy, injections, and analgesic medications. Based upon these findings and following a shared decision discussion with the patient that included outlining the risks of the procedure, a decision was made to proceed with knee replacement surgery.
Special Considerations
Patient selection for a Mako robot-assisted TKA depends largely on the judgement of the surgeon. Things to consider include sufficient articulation and range of motion of the ipsilateral hip in order to complete bone registration; the presence of metal in the operative leg, possibly creating artifacts in the CT scan that could reduce accuracy and adversely affect the operative plan; and the surgeon’s comfort level with using the Mako. At this time, only certain implants are compatible with the Mako robot, so additional factors need to be carefully considered. They include poor bone quality affecting stability of the implant; poor soft tissue integrity preventing restoration of a stable joint with the compatible implants; and the type and significance of the overall deformity in the knee, including flexion contractures and fixed varus/valgus alignment.
Discussion
Osteoarthritis is the most common joint disease. An estimated 37.4% of adults over the age 60 have radiographic evidence of arthritis.1 The projected number of total knee replacements, according to the US Census Bureau, is projected to increase by 3.5 million surgeries by 2030.2
TKA, in general, has produced excellent clinical outcomes over the past few decades.3, 4 Nevertheless, there is room for improvement. Studies show mechanical axis malalignment of more than 3 degrees in up to 31.8% of conventional TKAs versus 9% of computer-assisted TKAs.5 One of the largest factors determining good clinical outcomes is proper component placement.6, 7 In one cadaveric study, the average final bone cuts and component position were 5 and 3.1 times more precise with Mako TKA when compared to conventional TKA controls.8 Therefore, robotic-assisted total knee arthroplasty (RATKA) may increase the accuracy of bone cuts and component placement.
In another cadaveric study, Mako technology for RATKA demonstrated good soft tissue protection, including no injuries to the LCL, MCL, PCL, or patella tendon. This study also demonstrated that tibial subluxation and patellar eversion were not required for proper visualization while performing bone cuts.9
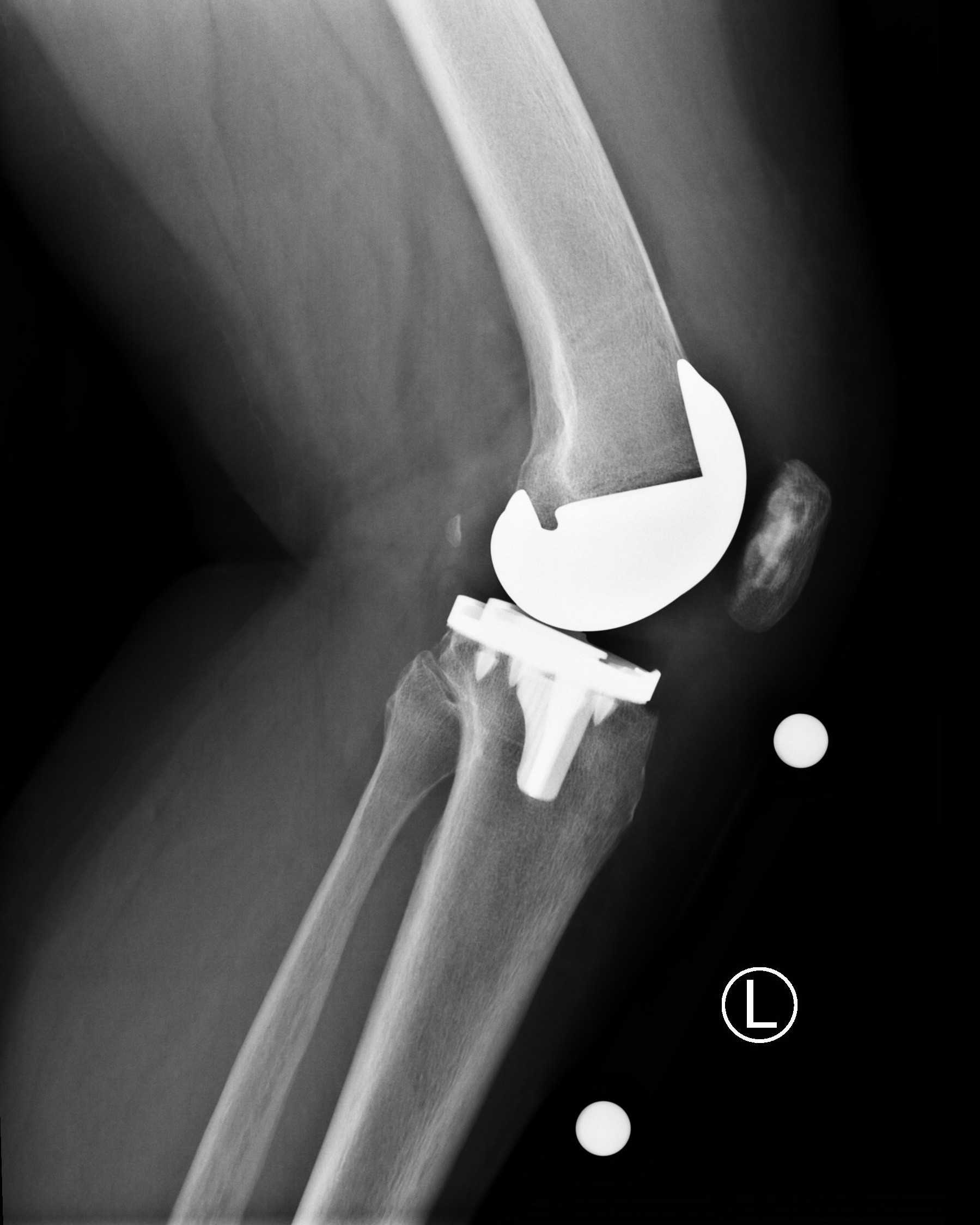
Although other robotic assisted systems exist, the Stryker Mako system was used in this case presentation with a Stryker Triathlon implant. The Triathlon total knee implant has demonstrated excellent survivorship of 99% in a ten-year follow-up study.10 There have been over 2 million Triathlon knees implanted, demonstrating that it is a reliable system that is now fully compatible with the Mako robotic-assisted technology.10
The broad spectrum of disease in arthritic knees and every patient’s unique anatomy can present challenges to the surgeon in performing a TKA. RATKA technology allows the surgeon to make intraoperative decisions using a live feedback loop based on preoperative 3D CT-based templating that allows for small adjustments in bone cuts and implant placement. The robotic arm technology, including real time feedback, allows the surgeon to balance the joint based on soft tissue tension before making bone cuts. In a single-surgeon study, Marchand et al. looked at intraoperative balancing and bony resection data for over 100 knees.11 They noted that all preoperative plans were adjusted intraoperatively, regardless of the degree of arthritic disease or the type of knee deformity. The intraoperative adjustments were able to achieve balance within a 1-mm difference between medial and lateral gaps in flexion in 97% of knees and extension in 100% of knees.12 Furthermore, the majority of knees did not require soft tissue releases for balancing.12 The ability to predict joint balancing and adjust component position prior to making bone cuts results in a balanced resection technique augmented with robotic-assisted technology for precision.
Another factor in determining good clinical outcomes in TKA surgery is using proper implant sizes.13 Although not always necessary, preoperative planning can help estimate the proper implant size.14 The RATKA technology is based on a preoperative 3D CT based template that allows the surgeon to accurately predict implant size. Bhimani et al. looked at 54 consecutive patients who underwent RATKA with the Mako RATKA system that provided a preoperative implant size template. Changes in implant size were made intraoperatively based on factors such as avoidance of femoral notching, avoidance or minimization of implant overhang, and maximization of cortical contact. The study demonstrated the software predicted the exact component size of 96% of the femoral components and 89% of the tibial components, and no template was off by more than 1 size.15 Furthermore, there were no cases of notching or implant overhang on either the femoral component or tibial component.15 Other studies have shown implant size templating to be 43.6% to 68% accurate using standard radiographs, explaining the practice is not common.16, 17
As with almost all new surgical techniques, there is a learning curve with RATKA. Sodhi et al. assessed the learning curve with RATKA and found that a surgeon can become comfortable with the technology to the point of not adding any operative time within a few months.18
Some studies have reported significantly lower mean pain scores, better overall physical function scores, greater patient satisfaction and clinical outcomes, and lower Forgotten Joint Scores in RATKA patients when compared with conventional manual TKA using a variety of patient-reported outcome measures.19, 20 Although studies with longer-term outcomes and larger populations are needed with this relatively new technology, early clinical outcomes are promising.
Equipment
Special equipment used in this surgery includes the Mako TKA System by Stryker.
Disclosures
We have nothing to disclose.
Statement of Consent
The patient referred to in this video article has given their informed consent to be filmed and is aware that information and images will be published online.
Citations
- Dillon CF, Rasch EK, Gu Q, Hirsch R. Prevalence of knee osteoarthritis in the United States: arthritis data from the Third National Health and Nutrition Examination Survey 1991-94. J Rheumatol. 2006;33:2271-2279.
- AAOS Total Knee and Hip Replacement Projections 2030. http://www.prnewswire.com/news-releases/total-knee-and-hip-replacement-surgery- projections-show-meteoricrise-by-2030-55519727.html. Accessed 17 September 2019.
- Jauregui JJ, Cherian JJ, Pierce TP, Beaver WB, Issa K, Mont MA. Long-term survivorship and clinical outcomes following total knee arthroplasty. J Arthroplasty. 2015;30:2164-6. doi:10.1016/j.arth.2015.05.052.
- National Joint Registry (NJR) for England, Wales, Northern Ireland and the Isle of Man. 13th Annual Report. Available at: https://reports.njrcentre.org.uk/. Accessed 17 September 2019.
- Sikorski GM. Computer-Assisted Surgery and Rotational Alignment of Total Knee Arthroplasty. In Total Knee Arthroplasty 2005 (pp. 254-257). Springer, Berlin, Heidelberg.
- Hernigou P, Deschamps G. Posterior slope of the tibial implant and the outcome of unicompartmental knee arthroplasty. J Bone Joint Surg Am. 2004 Mar;86(3):506-11. doi:10.2106/00004623-200403000-00007.
- Ulrich SD, Seyler TM, Bennett D, et al. Total hip arthroplasties: what are the reasons for revision? Int Orthop. 2008;32:597-604. doi:10.1007/s00264-007-0364-3.
- Hampp EL, Chughtai M, Scholl LY, et al. Robotic-arm assisted total knee arthroplasty demonstrated greater accuracy and precision to plan compared with manual techniques. J Knee Surg. 2019;32:239-50. doi:10.1055/s-0038-1641729.
- Bukowski BR, Anderson P, Khlopas A, Chughtai M, Mont MA. Improved functional outcomes with robotic compared with manual total hip arthroplasty. Surg Technol Int. 2016;29:303-8.
- Mistry JB, Elmallah RK, Chughtai M, Oktem ME, Harwin S, Mont M. Long-term survivorship and clinical outcomes of a single radius total knee arthroplasty. Surg Technol Int. 2016;28:247-51.
- Marchand RC, Bhowmik-Stoker M, Scholl L, Rodriquez L. Balanced Resection Surgical Technique for Robotic-Arm Assisted Total Knee Arthroplasty. AOA Annual Meeting, Oct 8-12, 2017, Adelaide, Australia.
- Marchand R, Bhowmik-Stoker M, School L, Rodriquez L. Balanced resection surgical technique for robotic-assisted total knee arthroplasty. Abstract AOA Annual Meeting, Oct 8-12,2017, Adelaide, Australia.
- Gonzalez MH, Mekhail AO. The failed total knee arthroplasty: evaluation and etiology. J Am Acad Orthop Surg. 2004;12:436–46. doi:10.5435/00124635-200411000-00008.
- Hernandez-Vaquero D, Abat F, Sarasquete J, Monllau JC. Reliability of preoperative measurement with standardized templating in total knee arthroplasty. World J Orthop. 2013;4:287-90. doi:10.5312/wjo.v4.i4.287.
- Bhimani S, Bhimani R, Feher A, Malkani A. Accuracy of preoperative implant sizing using 3D preplanning software for robotic-assisted total knee arthroplasty. AAHKS 2017 Annual Meeting. 2-5 Nov 2017. Dallas, TX.
- Ettiger M, Claassen L, Paes P, Calliess T. 2D versus 3D templating in total knee arthroplasty. Knee. 2016;23:149-151. doi:10.1016/j.knee.2015.08.014.
- Trickett RW, Hodgson P, Forster MC, Robertson A. The reliability and accuracy of digital templating in total knee replacement. J Bone Joint Surg Br. 2009;9:903-6. doi:10.1302/0301-620X.91B7.21476.
- Sodhi N, Khlopas A, Piuzzi NS, et al. The learning curve associated with robotic total knee arthroplasty. J Knee Surg. 2018;31:017-21. doi:10.1055/s-0037-1608809.
- Marchand RC, Sodhi N, Khlopas A, et al. Patient satisfaction outcomes after robotic-arm assisted total knee arthroplasty: a short-term evaluation. J Knee Surg. 2017;30:849-853. doi:10.1055/s-0037-1607450.
- Clark G. Australian Experience Mako Robotic TKA. AOA Annual Meeting, Oct 8-12, 2017, Adelaide.