Less Invasive Stabilization System (LISS) for Distal Femur Fracture Repair
Abstract
Distal femur fractures can occur in both high- or low-energy settings, and, in the latter, they are often associated with fragility fractures, such as in elderly or osteoporotic patients. In fragility fractures, poor bone quality can make adequate reduction challenging. Diagnosis is typically made with imaging, and obtaining both x-ray and computed tomography is crucial for adequate evaluation of fracture pattern and pre-procedural planning.
In this case, a displaced intra-articular distal femoral fracture was seen. An open reduction and internal fixation (ORIF) was used with an anterolateral approach to visualize the joint surface and obtain anatomic reduction of the articular surface. Then, a lateral lock plate was placed percutaneously to bridge the area of comminution while restoring leg length, alignment, and rotation.
Case Overview
Focused History
The patient is an 81-year-old man with significant dementia who had a total hip arthroplasty placed one year ago for the treatment of an intertrochanteric hip fracture. The patient sustained an unwitnessed fall out of bed at his assisted living facility. He is unable to recall what happened due to his dementia.
Tips for History:
What is the patient’s mechanism of injury?
High-energy mechanisms are more common in the younger population, including motor vehicle accidents and falls from height. Low-energy mechanisms are more common in the elderly and osteoporotics, including falls from standing.
Physical Exam
The patient's vital signs were stable. The left lower extremity had a superficial abrasion over the right proximal tibia, and there was swelling with deformity about the distal thigh. He had an intact neurovascular exam without evidence of an open wound.
Tips for Physical Exam:
- What is the patient’s ambulatory status? With distal femur fractures, the patient will typically be unable to ambulate due to pain.
- What deformity is apparent at the knee? Look for swelling and deformity at the distal thigh and knee.
- Assess distal neurovascular status. Assess vascular status by checking dorsalis pedis, posterior tibialis, and popliteal pulses. Lack of pulses compared to the contralateral limb may indicate a ruptured vessel. Test motor function of gastro/soleus, tibialis anterior, extensor hallucis longus, and flexor hallucis longus. Test sensory function of the lower limb.
- For any open distal femoral fracture, inject the knee with 120 cc of saline to rule out communication with the joint.
- Carefully examine the hip, knee, and ankle of the injured limb.
Imaging
It is important to obtain anteroposterior (AP) and lateral views of the complete femur, an AP pelvis, and 45-degree oblique views of the distal femur. If necessary, a traction view may help to evaluate the fracture pattern. Contralateral femoral views will be helpful for assessing the injured limb and for pre-procedural planning. Fractures that may involve the articular surface of the distal femur should be imaged with computed tomography (CT) for adequate evaluation of fracture pattern and pre-procedural planning. Additional CT angiography (CTA) may be necessary to evaluate vascular status in the setting of knee dislocation or abnormal vascular exam. Magnetic resonance imaging (MRI) may be beneficial for evaluating the soft tissue structures about the knee that may have been damaged during the femoral injury.
Natural History
Distal femur fractures, occurring in the distal third of the femur, make up four percent of all femoral fractures. The mechanism is typically related to high- or moderate-energy trauma, though they may occur as a result of a simple mechanical fall in elderly or osteoporotic patients. Treated non-surgically in traction, distal femur fractures may be complicated by infection, re-fracture, or nonunion.
Options for Treatment
- Non-operative using an unlocked Bledsoe brace: Consider for poor surgical candidates.
- 95-degree condylar blade plate (CBP): This option is technically challenging, making it a challenging option for simple femur fractures. Consider for complex proximal or distal femur fractures.
- Dynamic condylar screw (DCS): Introduced as an alternative to the CBP with a screw replacing the blade plate. This device requires only two-plane alignment, rather than the three-plane alignment necessary with the CBP. Insertion can be achieved by either standard lateral approach for direct reduction or by minimally invasive percutaneous approach for indirect reduction of extra-articular proximal or distal femur fractures. Minimally invasive approaches reduce soft tissue elevation and improve fracture healing rates, decrease infection, re-fracture, and the need for bone grafting techniques. Additionally, this method is compatible with total hip prostheses.
- Lateral locking plates (LLP): Unicortical LLPs are preferable in periarticular femur fractures with metaphyseal comminution. They may be used with the standard lateral or minimally invasive approaches. This strategy employs the concept of biological fixation, minimizing disruption to arterial supply, particularly the endosteal arteries in comparison with bicortical plating. Minimally invasive LLPs have been shown to be compatible with total knee arthroplasty as well as complex intra-articular fractures or in osteoporotic bone.
- Intramedullary nails (IMN): Retrograde IMNs have been demonstrated to be a successful strategy for treating supracondylar and intracondylar distal femur fractures. Antegrade IMNs have also been shown to be compatible in distal femur fractures following total knee arthroplasty, but are likely technically more challenging.
- External fixation: Consider external fixation to manage soft tissue injuries in open fractures, in multiply traumatized patients or those with severe burns or head injuries, in floating knees, or in infected femoral nonunions and pseudarthroses.
Special Considerations and Contraindications to Less Invasive Stabilization System (LISS)
The LISS plate provides multiple options for screw angles and lengths. In pre-operative planning, the surgeon may use referenced lengths based on cadaveric averages or may use a Kirschner wire to measure the screw length directly from the patient.6 Contraindications include poor surgical candidates and infections at the surgical site.
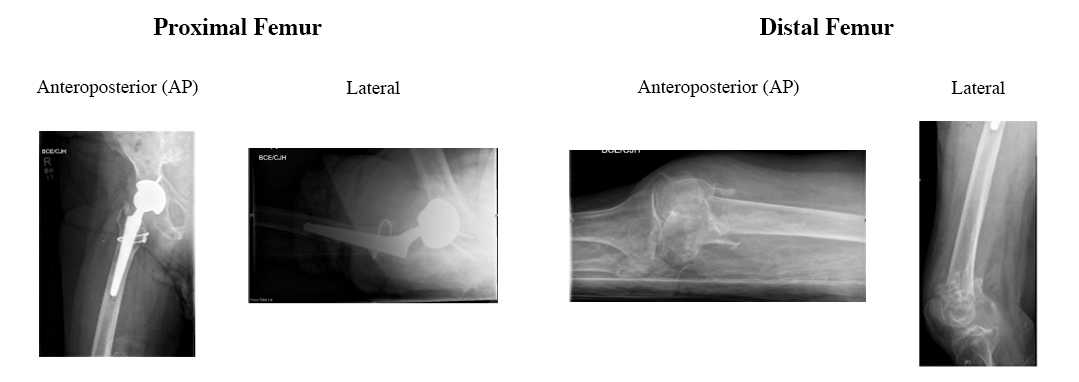
Pre-op X-Rays
Pre-operative Anterioposterior (AP) and Lateral views of the proximal and distal femur demonstrate an intact THA prosthesis and a comminuted, impacted fracture of the distal femur.
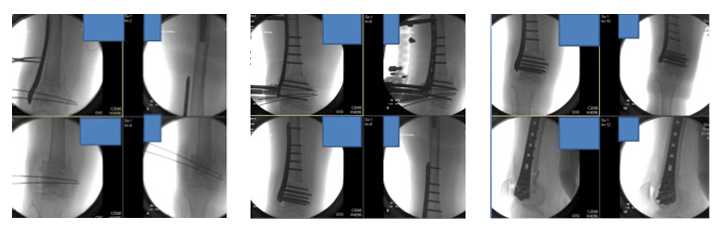
Intra-operative Fluoroscopy Images
Intra-operative fluoroscopic images show initial provisional reduction and final reduction with LISS plate fixation.
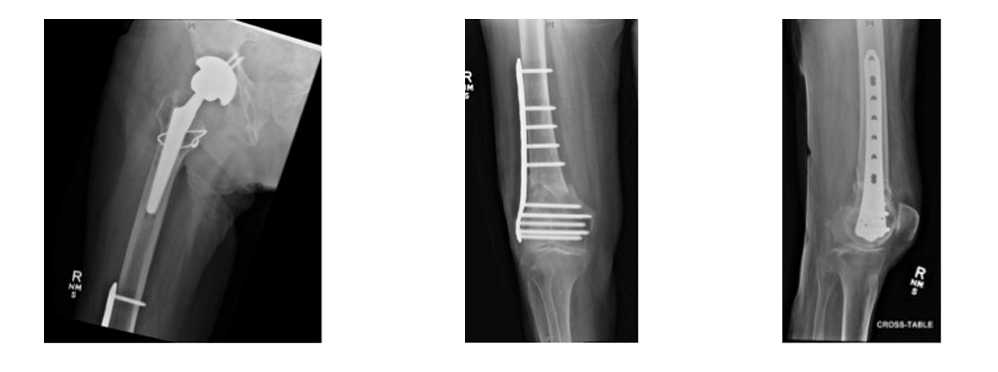
Post-operative X-Rays
Discussion
Plate osteosynthesis has been the preferred technique for repair of diaphyseal, metaphyseal, and articular fractures of the distal femur.7 Recent studies have demonstrated that surgeons can avoid damaging blood supply to the extent that occurs with a traditional lateral approach to the distal femur by using minimally invasive plating techniques. Two cadaveric studies by Farouk and colleagues showed that a minimally invasive percutaneous approach causes less disruption to the femoral blood supply including intact perforating and nutrient arteries, and better periosteal and medullary perfusion when compared with the conventional plate osteosyntheses.
Minimally invasive bridge plating is effective in the setting of comminuted fractures. Indirect fracture reduction may be possible with traction alone, as the soft tissue envelope remains intact if the standard lateral approach is not employed. The use of isolated proximal and distal incisions allows for purchase in surrounding intact femur segments. The minimally invasive bridge plating system adheres to the principles of biologic plating with increased healing potential by avoiding vascular disruption and reduced rates of infection.5 Additionally, this approach does not require bone grafting, which may be used in the open fixation.4
The LISS allows for minimally invasive submuscular plating with multiple screw fixations. Following indirect reduction, the plate is affixed to the lateral aspect of the femur. It acts in the manner of a definitive internal fixator to hold the reduced fracture in position. The locked internal fixator is not tightened against the bone so as to compress the periosteum, but maintains the alignment of the reduction and allows for relative stability and secondary healing.6 The plate design is anatomically shaped, based on femoral CT data and trials to maximize the best fit for the most femora. Screw angle options were optimized to allow condylar fixation without penetrating the intercondylar notch or patellofemoral joint. In comparison with the condylar blade plate and dynamic condylar screw, the LISS plate demonstrates stiffness and fatigue ratings that fall between these two implants. Biomechanical testing has demonstrated axial load strength superior to the condylar blade plate and retrograde intramedullary nail, and torsional strength that are inferior to these designs. The advantage of the LISS plate is its specific development for minimally invasive insertion with use of an insertion jig that allows easy screw targeting. Time to union, knee range of motion, and total complications were equivalent in a comparison of the LISS plate and the minimally invasive DCS construct, while the LISS plate demonstrated a lower rate of early implant failure.
In the setting of periprosthetic proximal and distal femur fracture repair, the variety of screw angle options in the LISS plate allows for optimal fixation around total hip or knee arthroplasty. 8 In addition, the plate has proven to be biomechanically sufficient in osteoporotic bone and clinically demonstrates no loss of condylar fixation in elderly patients. 19
Overall Outcomes After LISS Plate
Outcomes using a minimally invasive percutaneous approach with a lateral locking plate for supracondylar and intracondylar fractures are similar or superior to standard open approaches without the morbidity associated with extensive dissection or the need for bone grafting.4, 20 Use of the biologic plating concept has demonstrated early consolidation, lower infection and nonunion rates compared with the standard open technique. 15 Further, LISS plating has been shown to be effective when used for the treatment of periprosthetic proximal and distal femur fractures and high energy, mechanically unstable fractures.18, 21 The LISS plate promotes early mobilization and maintenance of knee range of motion following distal femur fracture fixation.
Future Research
A recent development in minimally invasive plating systems allows for polyaxial screw locking for a greater variety of screw angles. An early study of the Non-Contact Bridging-Distal Femur (NCB-DF) plate demonstrated better functional and radiographic outcomes compared with the LISS plate. Further research is necessary to see if the polyaxial locking plate will provide superior clinical outcomes compared with the monoaxial locking plate at long-term follow-up.
Patient Follow-Up
The patient followed up in the clinic one month after the operation. He was residing in rehab and remained in his knee immobilizer. He has been undergoing physical therapy. X-rays demonstrate interval callus formation across the fracture site and the hardware is intact without evidence of complication.
Equipment
Synthes LISS plate and screw construct (Synthes, Inc. USA)
Disclosures
The authors have no financial interests or conflict of interest to disclose.
Statement of Consent
The patient referred to in this video article has given their informed consent to be filmed and is aware that information and images will be published online.
Citations
- Egol KA, Koval KJ, Zuckerman JD. Handbook of Fractures. Philadelphia, PA: Lippincott Williams & Wilkins; 2010.
- Kolmert L, Wulff K. Epidemiology and treatment of distal femoral fractures in adults. Acta Orthop Scand. 1982;53(6):957-962. doi:10.3109/17453678208992855.
- Merchan EC, Maestu PR, Blanco RP. Blade-plating of closed displaced supracondylar fractures of the distal femur with the AO system. J Trauma. 1992;32(2):174-178. doi:10.1097%2F00005373-199202000-00010.
- Krettek C, Schandelmaier P, Miclau T, Tscherne H. Minimally invasive percutaneous plate osteosynthesis (MIPPO) using the DCS in proximal and distal femoral fractures. Injury. 1997;28(suppl 1):A20-A30. doi:10.1016/S0020-1383(97)90112-1.
- Haidukewych GJ. Innovations in locking plate technology. J Am Acad Orthop Surg. 2004;12(4):205-212. https://journals.lww.com/jaaos/Abstract/2004/07000/Innovations_in_Locking_Plate_Technology.1.aspx.
- Less invasive stabilization system (LISS): allows percutaneous plate insertion and targeting of screws in the distal femur. Technique guide. DePuy Synthes website. http://synthes.vo.llnwd.net/o16/LLNWMB8/US%20Mobile/Synthes%20North%20America/Product%20Support%20Materials/Technique%20Guides/SUTGLISSDistFemurJ2892H.pdf. Accessed February 21, 2015.
- Miclau T, Martin RE. The evolution of modern plate osteosynthesis. Injury. 1997;28(suppl 1):A3-A6. doi:10.1016/S0020-1383(97)90109-1.
- Kregor PJ, Hughes JL, Cole PA. Fixation of distal femoral fractures above total knee arthroplasty utilizing the Less Invasive Stabilization System (L.I.S.S.). Injury. 2001;32(suppl 3):64-75. doi:10.1016/S0020-1383(01)00185-1.
- Iannacone WM, Bennett FS, DeLong WG Jr, Born CT, Dalsey RM. Initial experience with the treatment of supracondylar femoral fractures using the supracondylar intramedullary nail: a preliminary report. J Orthop Trauma. 1994;8(4):322-327. doi:10.1097%2F00005131-199408000-00008.
- Ritter MA, Keating EM, Faris PM, Meding JB. Rush rod fixation of supracondylar fractures above total knee arthroplasties. J Arthroplasty. 1995;10(2):213-216. doi:10.1016/S0883-5403(05)80130-5.
- Alonso J, Geissler W, Hughes JL. External fixation of femoral fractures: indications and limitations. Clin Orthop Relat Res. 1989;241:83-88. https://journals.lww.com/clinorthop/Abstract/1989/04000/External_Fixation_of_Femoral_Fractures_.10.aspx.
- Farouk O, Krettek C, Miclau T, Schandelmaier P, Guy P, Tscherne H. Minimally invasive plate osteosynthesis and vascularity: preliminary results of a cadaver injection study. Injury. 1997;28(suppl 1):A7-A12. doi:10.1016/S0020-1383(97)90110-8.
- Farouk O, Krettek C, Miclau T, Schandelmaier P, Guy P, Tscherne H. Minimally invasive plate osteosynthesis: does percutaneous plating disrupt femoral blood supply less than the traditional technique? J Orthop Trauma. 1999;13(6):401-406. doi:10.1097%2F00005131-199908000-00002.
- Wenda K, Runkel M, Degreif J, Rudig L. Minimally invasive plate fixation in femoral shaft fractures. Injury. 1997;28(suppl 1):A13-A19. doi:10.1016/S0020-1383(97)90111-X.
- Krettek C, Müller M, Miclau T. Evolution of Minimally Invasive Plate Osteosynthesis (MIPO) in the femur. Injury. 2001;32(suppl 3):14-23. doi:10.1016/S0020-1383(01)00180-2.
- Stover M. Distal femoral fractures: current treatment, results and problems. Injury. 2001;32(suppl 3):3-13. doi:10.1016/S0020-1383(01)00179-6.
- Frigg R, Appenzeller A, Christensen R, Frenk A, Gilbert S, Schavan R. The development of the distal femur Less Invasive Stabilization System (LISS). Injury. 2001;32(suppl 3):24-31. doi:10.1016/S0020-1383(01)00181-4.
- Schuetz M, Müller M, Krettek C, et al. Minimally invasive fracture stabilization of distal femoral fractures with the LISS: a prospective multicenter study. Results of a clinical study with special emphasis on difficult cases. Injury. 2001;32(suppl 3):48-54. doi:10.1016/S0020-1383(01)00183-8.
- Zlowodzki M, Williamson S, Cole PA, Zardiackas LD, Kregor PJ. Biomechanical evaluation of the less invasive stabilization system, angled blade plate, and retrograde intramedullary nail for the internal fixation of distal femur fractures. J Orthop Trauma. 2004;18(8):494-502. doi:10.1097/00005131-200409000-00004.
- Zlowodzki M, Williamson S, Zardiackas LD, Kregor PJ. Biomechanical evaluation of the less invasive stabilization system and the 95-degree angled blade plate for the internal fixation of distal femur fractures in human cadaveric bones with high bone mineral density. J Trauma. 2006;60(4):836-840. doi:10.1097/01.ta.0000208129.10022.f8.
- Kao FC, Tu YK, Su JY, Hsu KY, Wu CH, Chou MC. Treatment of distal femoral fracture by minimally invasive percutaneous plate osteosynthesis: comparison between the dynamic condylar screw and the less invasive stabilization system. J Trauma. 2009;67(4):719-726. doi:10.1097/TA.0b013e31819d9cb2.
- Kobbe P, Klemm R, Reilmann H, Hockertz TJ. Less invasive stabilisation system (LISS) for the treatment of periprosthetic femoral fractures: a 3-year follow-up. Injury. 2008;39(4):472-479. doi:10.1016/j.injury.2007.10.034.
- Kregor PJ, Stannard JA, Zlowodzki M, Cole PA. Treatment of distal femur fractures using the less invasive stabilization system: surgical experience and early clinical results in 103 fractures. J Orthop Trauma. 2004;18(8):509-520. doi:10.1097/00005131-200409000-00006.
- Krettek C, Schandelmaier P, Miclau T, Bertram R, Holmes W, Tscherne H. Transarticular joint reconstruction and indirect plate osteosynthesis for complex distal supracondylar femoral fractures. Injury. 1997;28(suppl 1):A31-A41. doi:10.1016/S0020-1383(97)90113-3.
- Schütz M, Müller M, Regazzoni P, et al. Use of the Less Invasive Stabilization System (LISS) in patients with distal femoral (AO33) fractures: a prospective multicenter study. Arch Orthop Trauma Surg. 2005;125(2):102-108. doi:10.1007/s00402-004-0779-x.
- Kregor PJ, Stannard J, Zlowodzki M, Cole PA, Alonso J. Distal femoral fracture fixation utilizing the Less Invasive Stabilization System (L.I.S.S.): the technique and early results. Injury. 2001;32(suppl 3):32-47. doi:10.1016/S0020-1383(01)00182-6.
- Schandelmaier P, Partenheimer A, Koenemann B, Grün OA, Krettek C. Distal femoral fractures and LISS stabilization. Injury. 2001;32(suppl 3):55-63. doi:10.1016/S0020-1383(01)00184-X.
- Weight M, Collinge C. Early results of the less invasive stabilization system for mechanically unstable fractures of the distal femur (AO/OTA types A2, A3, C2, and C3). J Orthop Trauma. 2004;18(8):503-508. doi:10.1097/00005131-200409000-00005.
- Kolb W, Guhlmann H, Windisch C, Marx F, Kolb K, Koller H. Fixation of distal femoral fractures with the less invasive stabilization system: a minimally invasive treatment with locked fixed-angle screws. J Trauma. 2008;65(6):1425-1434. doi:10.1097/TA.0b013e318166d24a.
- Hanschen M, Aschenbrenner IM, Fehske K, et al. Mono- versus polyaxial locking plates in distal femur fractures: a prospective randomized multicentre clinical trial. Int Orthop. 2014;38(4):857-863. doi:10.1007/s00264-013-2210-0.