Bonebridge Implant
Abstract
Bone conduction implants can improve hearing in patients with conductive or mixed hearing loss as well as in cases of single-sided deafness (SSD). The Bonebridge implant has three components: a magnet, an internal transducer, and an external audio processor. The patient in this case previously underwent resection of a vestibular schwannoma via a middle fossa craniotomy in an attempt to preserve hearing. Unfortunately, the patient ultimately lost hearing in the right ear, resulting in SSD. Here, we demonstrate the step-by-step surgical technique for the Bonebridge implant to allow sound transmission from the patient’s deaf ear to the contralateral cochlea via bone conduction.
Case Overview
Background
Bone conduction implants are used in patients who have conductive or mixed hearing loss, as well as in cases of single-sided deafness. The Bonebridge device is an active transcutaneous bone conduction implant that has both internal and external components.1 The implanted portion consists of both a magnet and a bone conduction-floating mass transducer (BC-FMT), while the external component is an audio processor. The internal and external components are connected transcutaneously via a magnet, and a hearing aid battery powers the audio processor externally.1 This transcutaneous connection is unique in that there is no defect in the skin or soft tissue that is present with prior versions of bone conduction implants. The audio processor detects sound and transmits it to the implant via the magnet, which in turn vibrates within the bone, resulting in ‘active’ bone conduction of sound.1 The Bonebridge may be performed in patients over the age of five years (> 12 in the United States), who have conductive or mixed unilateral hearing loss that meets specific pure tone average threshold requirements.1, 2 Hearing loss in the affected side can be severe, but the contralateral ear should have a relatively normal hearing (bone conduction threshold above 20 dB from 500 Hz to 3 kHz). It is also indicated in patients who have conductive or mixed hearing loss and have a bone pure tone average less than or equal to 45 dB at 500 Hz, and 1, 2, and 3 kHz.2
Focused History of the Patient
This patient developed unilateral deafness after a middle fossa craniotomy for resection of a vestibular schwannoma.
Physical Exam
Hearing loss is grossly evaluated using the Weber and Rinne tests. These tests make use of a tuning fork to differentiate between conductive and sensorineural hearing loss.
The Weber test is performed by placing a vibrating tuning fork over the forehead or incisor at the midline. The patient is asked to identify on which side the vibrations are heard more loudly. If the patient has conductive hearing loss, the sound will localize to the impaired ear. If the patient has sensorineural hearing loss, the sound will localize to the better hearing ear, indicating a sensorineural hearing loss in the opposite ear.3, 4
The Rinne test is used to differentiate between sensorineural and conductive hearing loss. The test is performed by placing the vibrating tuning fork over the mastoid bone behind the ear (bone conduction) until the patient can no longer hear, and then quickly moving the tuning fork just lateral to the external auditory canal (air conduction). In patients with normal hearing or sensorineural hearing loss, air conduction will be perceived as louder than bone conduction. In patients with conductive hearing loss, the bone conduction will be greater than the air conduction.3, 4 The Rinne test can also be performed by placing the tuning fork on the mastoid and lateral to the EAC at separate times and asking at which location the patient perceives the sound to be louder.3, 4 These tests, however, are not without limitations, and there is substantial variation in their accuracy.5 Additionally, only a single frequency (typically 512 Hz) is tested.
The gold standard for diagnosis of hearing loss is by a pure-tone audiogram with appropriate masking techniques and word recognition scores. It differentiates between conductive and sensorineural hearing loss and also provides hearing threshold cutoffs that help to define the severity of the hearing loss and the frequencies of hearing that are most affected.6
Imaging
Computed tomography (CT) must be completed prior to Bonebridge implantation to assess for temporal bone suitability for implantation of the BC-FMT and in order to rule out a retrocochlear pathology.1 Some surgeons elect to use 3D CT analysis to create a temporal bone well template. Others have even created 3D printed models of the temporal bone for planning in complex cases.7
Natural History
Unilateral hearing loss can be conductive, sensorineural, or mixed, and is differentiated by Weber and Rinne tests as well as an audiogram. Etiologies of conductive hearing loss are numerous and include otosclerosis, ossicular dislocation, superior semicircular canal dehiscence, congenital malformation, and middle ear effusion. Etiologies of sensorineural hearing loss include presbycusis, Meniere’s disease, infectious causes, and a retrocochlear pathology such as a vestibular schwannoma. Any patient that presents with unilateral or asymmetric sensorineural hearing loss requires further evaluation to detect any retrocochlear pathology. In the setting of these findings, an MRI is required to further evaluate and confirm the diagnosis.8 Surgical resection of a vestibular schwannoma can result in reduced or complete loss of hearing. The risk of this loss varies based upon the surgical approach. Both middle fossa craniotomy and retrosigmoid approaches allow for hearing preservation, but these rates vary widely and depend on both surgeon and patient/tumor factors.
Options for Treatment
Patients with SSD may be treated with a variety of devices. These range from hearing aids, bone conduction implants, and even cochlear implants. One option for patients with single-sided deafness is air conduction contralateral routing of signal (CROS) hearing aids. These devices route sound from the non-functioning ear to the functional ear. These devices, however, are only accepted by 10–20% of patients, with 80–90% of patients with unilateral hearing loss opting for bone conduction implant.2 SSD is also increasingly being treated with cochlear implant, with increasing evidence for its effectiveness and improvements in quality of life scores for patients.
The traditional type of bone conduction implant is the percutaneous, bone-anchored hearing aid (BAHA). These devices consist of an osseointegrated titanium screw and an abutment, which protrudes through the soft tissue and skin. While these devices are effective in the treatment of conductive/hearing loss and single-sided deafness, they are associated with complications such as infection around the titanium screw, skin overgrowth, and wound dehiscence.9
These complications are more likely to occur with percutaneous devices compared with transcutaneous devices that do not communicate with an outside environment. The advantages of the Bonebridge include improved cosmesis and earlier activation time (2–4 weeks) as the device does not require osseointegration.1 There are no significant differences between the two devices for functional gain and word recognition scores.9, 10
Passive bone conduction devices rely on the vibration of the skin and soft tissue and do not vibrate the bone directly. Like the Bonebridge, they are transcutaneous, but the sound is captured from the environment and transformed into an electrical signal that then stimulates the magnet and does not directly stimulate the bone of the skull.11 One study compared the passive and active devices and found that there were similar cutaneous complications with transcutaneous as the BAHA.
Rationale for Treatment
This patient had SSD, one of the three primary indications for Bonebridge placement.
The ideal outcome of her surgery would be a noticeable improvement in her ability to hear. One review study found that the patients, with conductive or mixed loss hearing and were treated with the Bonebridge implant, had a functional gain from 24 to 37 dB, which was stable over time.1, 2
Single-sided deafness is the newest indication for Bonebridge implantation, and there are fewer studies that evaluate outcomes in these patients. However, the smaller studies that have been completed demonstrate improved speech recognition in both quiet and noisy environments.12
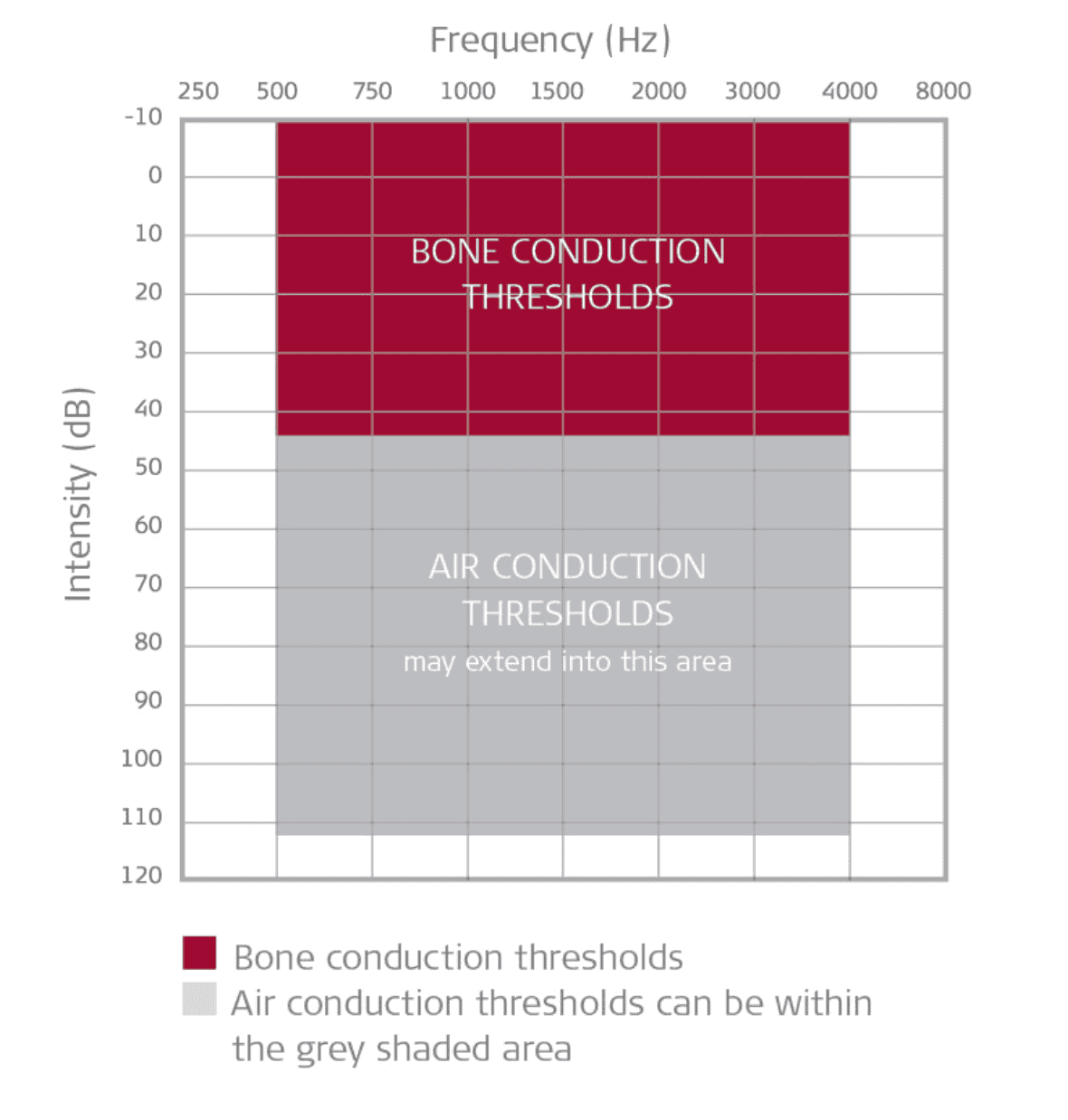
Figure 1: Audiological criteria for Bonebridge.
Special Considerations
In addition to an age requirement, patients should have conductive, mixed, or unilateral hearing loss that meet the previously defined pure tone average threshold requirements.1, 2 Patients with ear canal atresia have been shown to benefit substantially as they have a large air-bone gap with a preserved inner ear mechanism. Similarly, patients with otosclerosis, ear canal stenosis, or a chronic draining ear that prevents usage of traditional hearing aids, will also benefit.1, 2
After Bonebridge implantation, patients will have a large artifact on MRI that significantly affects the ability to assess both the ipsilateral as well as the contralateral cranial vaults.13
Discussion
Single-sided deafness was added to the list of indications for bone conduction implants in the 2000s.2 The development of transcutaneous bone conduction implants such as the Bonebridge implant allowed for substantial reductions in complications associated with the more traditionally used percutaneous models, which have been in use since the 1970s.2, 9 The Bonebridge device was first implanted in 2011.2
The procedure can be done under either local or general anesthesia.1 Approaches include a mastoid, retrosigmoid, or middle fossa placement. For the mastoid approach, a standard postauricular incision is performed. Exposure of both the posterior canal and the mastoid cortex should be accomplished. These landmarks, along with the temporal line, will help to identify the sinodural angle, which is the ideal site for implantation of the BC-FMT.2 Care is then taken to measure where the device will sit within the mastoid. Preoperative assessment with CT can assist in ensuring appropriate location planning. The site is then prepared for the implant using a drill. The drill depth is determined by the patient’s anatomy. In cases where the patient has a thin mastoid (i.e. dura or sigmoid in close proximity), a lift may be necessary in order to avoid compression of these structures. A lift is a thin washer that can be attached to the wings of the BC-FMT, ranging from 1–4 mm in thickness.2 A subperiosteal pocket is created adjacent to the drilled site in the mastoid to accommodate the coil portion of the device, similar to site preparation for a cochlear implant receiver/stimulator. Two pilot holes are then created with the drill bit that is included in the Bonebridge kit. The BC-FMT is secured with two screws, and the wound is subsequently closed in layers.
The surgery lasts less than an hour, with minimal blood loss, and is performed on an outpatient basis. The cosmetic result is excellent as the incision is hidden behind the ear. There are no permanent external components compared with percutaneous models.1 An external device is connected via a magnet to allow for the conduction of signals from the external environment.
The Bonebridge provides substantial benefit to patients, with improved hearing outcomes and relatively few complications.2 Adverse events after implantation are rare, but include pain, dizziness, tinnitus, or minor skin infections. These complications typically resolve within a few days with medical management.2 Patients with SSD typically note improvements in speech recognition in quiet and noisy environments, both objectively and subjectively. Patients are also found to be generally satisfied with their devices.2
The Bonebridge implant continues to be a well-tolerated, safe, and effective option for the treatment of patients with unilateral, mixed, or conductive hearing loss.
Equipment
Stryker 5 diamond drill
Bonebridge implant kit
Disclosures
Nothing to disclose.
Statement of Consent
The patient referred to in this video article has given their informed consent to be filmed and is aware that information and images will be published online.
Citations
- Miller ME. Osseointegrated auditory devices: Bonebridge. Otolaryngol Clin North Am. 2019;52(2):265-272. doi:10.1016/j.otc.2018.11.006.
- Sprinzl GM, Wolf-Magele A. The Bonebridge bone conduction hearing implant: indication criteria, surgery and a systematic review of the literature. Clin Otolaryngol. 2016;41(2):131-143. doi:10.1111/coa.12484.
- Recommended procedure for Rinne and Weber tuning-fork tests. British Society of Audiology. Br J Audiol. 1987;21(3):229-230. doi:10.3109/03005368709076410.
- Sheehy JL, Gardner G, Hambley WM. Tuning fork tests in modern otology. Arch Otolaryngol. 1971;94(2):132-138. doi:10.1001/archotol.1971.00770070368009.
- Kelly EA, Li B, Adams ME. Diagnostic accuracy of tuning fork tests for hearing loss: a systematic review. Otolaryngol Head Neck Surg. 2018;159(2):220-230. doi:10.1177/0194599818770405.
- Davies RA. Audiometry and other hearing tests. Handb Clin Neurol. 2016;137:157-176. doi:10.1016/B978-0-444-63437-5.00011-X.
- Mukherjee P, Cheng K, Flanagan S, Greenberg S. Utility of 3D printed temporal bones in pre-surgical planning for complex BoneBridge cases. Eur Arch Otorhinolaryngol. 2017;274:3021-3028. doi:10.1007/s00405-017-4618-4.
- Reiss M, Reiss G. Zur differentialdiagnose der einseitigen schwerhörigkeit [Differential diagnosis of unilateral hearing loss]. Praxis (Bern 1994). 2000;89(6):241-247.
- Gerdes T, Salcher RB, Schwab B, Lenarz T, Maier H. Comparison of audiological results between a transcutaneous and a percutaneous bone conduction instrument in conductive hearing loss. Otol Neurotol. 2016;37(6):685-691. doi:10.1097/MAO.0000000000001010.
- Ihler F, Blum J, Berger MU, Weiss BG, Welz C, Canis M. The prediction of speech recognition in noise with a semi-implantable bone conduction hearing system by external bone conduction stimulation with headband: a prospective study. Trends Hear. 2016 Oct 3;20:2331216516669330. doi:10.1177/2331216516669330.
- Zernotti ME, Di Gregorio MF, Galeazzi P, Tabernero P. Comparative outcomes of active and passive hearing devices by transcutaneous bone conduction. Acta Otolaryngol. 2016;136(6):556-558. doi:10.3109/00016489.2016.1143119.
- Salcher R, Zimmermann D, Giere T, Lenarz T, Maier H. Audiological results in SSD with an active transcutaneous bone conduction implant at a retrosigmoidal position. Otol Neurotol. 2017;38(5):642-647. doi:10.1097/MAO.0000000000001394.
- Steinmetz C, Mader I, Arndt S, Aschendorff A, Laszig R, Hassepass F. MRI artefacts after Bonebridge implantation. Eur Arch Otorhinolaryngol. 2014;271(7):2079-2082. doi:10.1007/s00405-014-3001-y.


