Frontal Sinus Dissection (Cadaver)
Article Overview
The frontal sinus is a critical anatomical structure that frequently presents complex pathologies requiring advanced surgical intervention. Endoscopic frontal sinus surgery is a treatment method for a variety of conditions, including medically refractory chronic rhinosinusitis,1 mucocele,2,3 and neoplasms.4 Frontal sinus dissection (FSD) techniques, classified according to the Draf system, require a comprehensive understanding of the frontal sinus anatomy and the skilled execution of delicate surgical maneuvers.5 The frontal sinus recess is a complex three-dimensional structure that is significantly influenced by several neighboring anatomical features, including the agger nasi cells, frontal cells, nasal beak, anteromedial frontal sinus floor, attachment of the most anterior middle turbinate, and the nasal septum.6 Importantly, these surrounding structures exhibit a high degree of anatomical variability between individuals, presenting a substantial challenge for the operating surgeon. Frontal sinus structures are lined with a delicate mucosal lining, which adds complexity to surgical management. This mucosal lining plays a critical role in the normal physiological functioning and healing processes of both the frontal sinus and the entire nasal cavity. The preservation of this delicate mucosa is very important, as any unnecessary damage can lead to adverse outcomes, such as scarring and stenosis, which can significantly compromise the success of surgical interventions targeting the frontal sinus region. Complications arising from improper technique or unintended injury to critical structures, including the anterior ethmoid artery (AEA) and the cribriform plate, can also lead to severe consequences, underscoring the importance of thorough surgical planning and execution. Figure 1 illustrates a frontal sinus outflow tract on the sagittal CT scan.
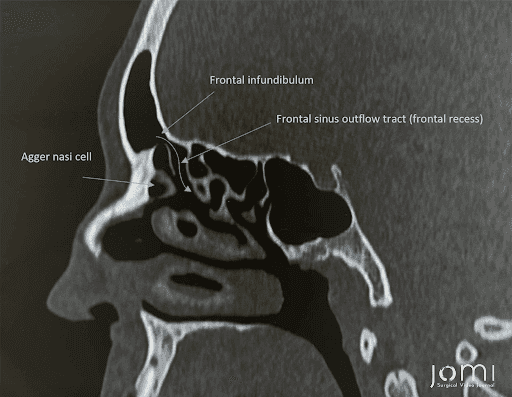
Figure 1. Frontal Sinus Outflow Tract on CT.
This cadaveric study aims to provide a detailed overview of the key steps involved in the dissection of the frontal sinus, including the identification of anatomical landmarks, performing of Draf I, II-A, II-B, and III procedures, and the preservation of mucosal structures.
The FSD procedure begins by transitioning to curved instruments to optimize access and maneuverability within the frontal sinus. Hyperextending the patient's head improves visualization and accessibility. Using a 45-degree endoscope, the key anatomical landmarks are identified, including the boundaries of the frontal sinus outflow tract or frontal infundibulum.
The frontal sinusotomy is classified according to the Draf system, with the Draf I procedure being the initial stage.7 This relies on a thorough anterior ethmoidectomy, removing anterior ethmoidal cells down to the skull base. The suprabullar cells and agger nasi are dissected to create working space and visualize the frontal sinus outflow tract while preserving the frontal sinus mucosa.
Following the crushing of the agger nasi, a clearer view of the frontal sinus is obtained. In the absence of navigation, transillumination can help confirm entry into the frontal sinus cavity. The Draf II sinusotomy is subdivided into two main approaches: Draf IIA and Draf IIB. The Draf IIA procedure, described as "uncapping the egg," results in complete exposure of the frontal ostium. This is achieved by removing any frontal cells occluding the frontal ostium and recess, primarily involving the removal of the superior portion of the agger nasi to facilitate access to the frontal sinus. The Draf IIA approach aims to provide unobstructed visualization and access to the frontal sinus.8 Upon completion of the Draf IIA procedure, the subsequent step involves progressing to a Draf IIB frontal sinusotomy, further expanding the surgical access to address frontal sinus pathologies comprehensively. The frontal sinusotomy is extended from the orbital roof towards the septum, necessitating the removal of the vertical lamella of the middle turbinate. Careful attention is paid to the location of the AEA, which typically runs approximately one centimeter behind the frontal outflow tract when it is below the skull base.9
The unilateral Draf IIB frontal sinus approach has limitations due to the septum and orbit. In situations where this approach does not provide sufficient width for a patent opening, extending the procedure to the contralateral side is appropriate. The Draf III procedure, which opens the frontal sinus floor from orbit to orbit, becomes the next surgical option in such cases. This procedure aims to create a wide, horseshoe-shaped cavity from orbit to orbit.10 Saucerization removes obstructing bony septations, and a superior anterior septectomy is performed to resect the perpendicular ethmoid plate. Throughout the procedure, cold dissection techniques are favored over drilling to minimize mucosal damage and preserve as much mucosa as possible. However, in some cases, opening into the contralateral frontal recess may be impossible or unnecessary. In these instances, the Draf IIC approach can be applied. This technique is an extension of the Draf IIB, involving the opening of the occluded frontal sinus through the midline without extending into the contralateral frontal recess. This approach is preferred in the presence of an interfrontal septal sinus or an eccentrically located frontal sinus septum.11
The complex and diverse nature of frontal sinus anatomy poses a significant challenge for clinicians, often making adequate visualization and access to the affected areas difficult to achieve. The proximity of the frontal sinus to vital structures, including the orbit and anterior cranial fossa, increases the risk of complications during surgery. This anatomical complexity, coupled with the predisposition of the frontal sinus to postoperative scarring and stenosis, underscores the importance of tailoring the surgical approach to the unique needs of each patient. Surgical navigation systems, which provide real-time, three-dimensional imaging, have become indispensable in addressing these challenges. It revolutionized frontal sinus surgery by enhancing precision, safety, and outcomes. They utilize advanced imaging techniques, such as computed tomography (CT) and magnetic resonance imaging (MRI), to create detailed anatomical maps. These maps guide surgeons in real-time, allowing for precise localization and navigation within the frontal sinus. This precision is crucial in avoiding critical structures and ensuring complete removal of diseased tissue.The use of surgical navigation significantly reduces the risk of iatrogenic injury to vital structures. By providing accurate spatial orientation, these systems help surgeons avoid the optic nerve, dura mater, and other critical areas. This is particularly important in the narrow and variable corridors of the frontal sinus, where even minor deviations can lead to severe complications. Clinical studies have demonstrated that surgical navigation improves surgical outcomes in frontal sinus surgery. These improvements include reduced intraoperative blood loss, shorter operative times, and lower rates of postoperative complications. Additionally, the precision offered by navigation systems decreases the likelihood of requiring revision surgeries, thereby enhancing overall patient outcomes. Surgical navigation is especially valuable in complex cases, such as those involving extensive sinus disease, tumors, or previous surgical interventions. In these scenarios, the detailed anatomical guidance provided by navigation systems is critical for thorough and safe removal of pathological tissue, minimizing the risk of residual disease and recurrence. Beyond its clinical applications, surgical navigation serves as an excellent educational tool. It allows trainees to visualize and understand the intricate anatomy of the frontal sinus, facilitating better learning and skill acquisition. This educational aspect is vital for the ongoing development of surgical expertise in otolaryngology.
To summarize, the video presented here serves as an invaluable resource for both practicing surgeons and medical students. For practicing surgeons, this resource provides a valuable reference for navigating the various stages of FSD, from the initial Draf I procedure to the more complex Draf II-A, II-B, and III techniques. The meticulous identification and preservation of crucial anatomical landmarks, such as the frontal sinus outflow tract, the agger nasi, and the vertical lamella of the middle turbinate, are essential for avoiding complications, including injury to the AEA or inadvertent penetration of the cribriform plate.
By familiarizing themselves with the step-by-step approach outlined in this text and the accompanying video, surgeons can enhance their technical proficiency and improve patient outcomes in the management of frontal sinus-related conditions. For medical students and trainees, this video offers an invaluable learning opportunity to develop a deep understanding of frontal sinus anatomy and the nuances of endoscopic dissection techniques. By using this knowledge, healthcare professionals can enhance their surgical skills, improve patient care, and contribute to the advancement of the field of endoscopic sinus surgery.
Duke University Cadaver Lab Series
Check out the rest of the series below:
Citations
- DeConde AS, Smith TL. Outcomes after frontal sinus surgery: an evidence-based review. Otolaryngol Clin North Am. 2016;49(4). doi:10.1016/j.otc.2016.03.024.
- Trimarchi M, Bertazzoni G, Bussi M. Endoscopic treatment of frontal sinus mucoceles with lateral extension. Ind J Otolaryngol Head Neck Surg. 2013;65(2). doi:10.1007/s12070-012-0611-9.
- Peng Z, Wang Y, Fang Y, et al. Precision endonasal endoscopic surgery of the frontal recess cells and frontal sinus guided by the natural sinus drainage pathway. Front Surg. 2022;9. doi:10.3389/fsurg.2022.862178.
- Banhiran W, Casiano RR. Endoscopic sinus surgery for benign and malignant nasal and sinus neoplasm. Curr Opin Otolaryngol Head Neck Surg. 2005;13(1). doi:10.1097/00020840-200502000-00012.
- Draf W. Endonasal micro-endoscopic frontal sinus surgery: the fulda concept. Operat Tech Otolaryngol Head Neck Surg. 1991;2(4). doi:10.1016/S1043-1810(10)80087-9.
- Dassi CS, Demarco FR, Mangussi-Gomes J, Weber R, Balsalobre L, Stamm AC. The frontal sinus and frontal recess: anatomical, radiological and surgical concepts. Int Arch Otorhinolaryngol. 2020;24(3). doi:10.1055/s-0040-1713923.
- Stucker FJ, De Souza C, Kenyon GS, Lian TS, Draf W, Schick B. Rhinology and Facial Plastic Surgery.; 2009. doi:10.1007/978-3-540-74380-4.
- Eviatar E, Katzenell U, Segal S, et al. The endoscopic Draf II frontal sinusotomy: non-navigated approach. Rhinol. 2006;44(2).
- Mohammed K, Komser A, Goldberg AN. Unilateral transnasal endoscopic approach to frontal sinuses: Draf IIc. Aller Rhinol. 2013;4(2). doi:10.2500/ar.2013.4.0058.
- Dubin MG, Kuhn FA. Endoscopic modified lothrop (Draf III) with frontal sinus punches. Laryngoscope. 2005;115(9). doi:10.1097/01.mlg.0000176542.59985.9f.
-
Gotlib T, Held-Ziółkowska M, Niemczyk K. Extended draf IIb procedures in the treatment of frontal sinus pathology. Clin Exp Otorhinolaryngol. 2015 Mar;8(1):34-8. doi:10.3342/ceo.2015.8.1.34.