Recipient Kidney Transplant from a Living Donor
Abstract
End stage renal disease (ESRD) is the final stage in the progression of chronic kidney disease (CKD). CKD has a multitude of etiologies, presents in a variety of ways, and progresses in a patient-dependent manner. Despite the heterogeneity of CKD, once ESRD ensues, patients require Renal Replacement Therapy (RRT). RRT is one of three prongs: hemodialysis, peritoneal dialysis, or kidney transplant. Of these, kidney transplantation provides the patient with the best quality of life, an improved survival, and an opportunity for cure. However, the success of kidney transplantation with improved outcomes and tolerance to the required immunosuppression has led to an extreme organ shortage despite the increase in deceased organ donors. As a result, the push for living donors has become increasingly more important. For recipients, the best outcomes are with transplants from a living donor due to superior graft quality and elimination of the need for waiting and dialysis. This article will present such a case and discuss the important considerations a physician must make preoperatively and intraoperatively when performing kidney transplantations.
Case Overview
Background
The National Kidney Foundation definition of chronic kidney disease (CKD) was established in order to standardize the approach to care for this patient population. CKD is defined as kidney damage for greater than or equal to 3 months by structural or functional abnormalities of the kidney and/or a glomerular filtration rate (GFR) of < 60 mL/min/1.73m2. The stages of CKD vary by GFR level: in stage I, GFR is ≥ 90; in stage II, GFR is 60–89; in stage III, GFR is 30–59; in stage IV, GFR is 15–29; and in stage V (kidney failure), GFR is < 15 or dialysis dependence.2 In this case report, we will discuss a patient with end stage renal disease (stage V CKD) who underwent living related kidney transplant prior to the initiation of dialysis.
Focused History of Patient
This patient is a 56-year-old female with a past medical history of type I diabetes mellitus, hypertension, hypothyroidism, hyperlipidemia and ESRD secondary to diabetic and hypertensive nephropathies who presented to the Massachusetts General Hospital for a living related kidney transplant from her sister.
Her past surgical history is significant for a cesarean section and left upper extremity AV fistula. Her notable medications include amlodipine, calcitriol, levothyroxine, olmesartan, pravastatin, lasix, and kayexalate. She is allergic to aspirin and penicillin. Socially, the patient lives with her husband and teaches in a local elementary school. She has a vaccinated dog and a turtle as pets but notes she will no longer care for her turtle following transplant. She does not drink alcohol and was a former smoker with a 1 pack-year history, quitting in 1979. She denies any illicit drug use. She denies any recent travel or tuberculosis exposure in her past.
Physical Exam
On preoperative exam the patient was noted to be a well-appearing 56-year-old female. Her abdominal exam was noted to be within normal limits with a soft, non-distended abdomen and a well-healed surgical incision from her cesarean section. Her femoral and pedal pulses were palpable bilaterally. In a patient with ESRD that is being considered for renal transplant, it is important to assess the lower extremity pulses for evidence of significant peripheral vascular disease. This is to ensure minimal atherosclerotic disease where the transplanted kidney’s artery will be anastomosed on the recipient’s iliac vessels. Any significant peripheral arterial disease (PAD) in the aortoiliac system could compromise circulation to the allograft or to the ipsilateral lower extremity due to dissection in the iliofemoral arteries distally, or it could steal from the lower extremity circulation by the allograft.2
Imaging Studies
In general, cardiac evaluation prior to kidney transplantation includes: EKG and echocardiography. Additionally, a stress test and/or coronary angiography is conducted for inpatients with history of CAD or significant risk factors (diabetes mellitus, hemodialysis for greater than one year, left ventricular hypertrophy, age of > 60 years, smoking history, hypertension, or hyperlipidemia). In patients with symptoms or signs of voiding abnormalities or urinary obstruction (e.g. prostatic), a voiding cystourethrogram and complete lower urinary tract evaluation is necessary to rule out outlet obstruction.3 If the patient has any history of peripheral vascular disease or any concerning findings on vascular exam, the patient should undergo pulse volume recordings (PVRs) of the lower extremities and/or a CT scan of the abdomen and pelvis (without contrast) to assess for iliac calcifications.
This patient underwent preoperative EKG that showed no arrhythmia or ischemia. However, given that her past medical history included several coronary artery disease (CAD) risk factors, she underwent coronary angiography that excluded severe atherosclerotic lesions. A preoperative chest x-ray showed evidence of prior granulomatous disease, and a follow up chest CT scan confirmed this without other concerning findings (Figures 1–3).
Additionally, her donor sister underwent the standard donor preoperative work up. This includes assuring adequate renal function and minimal risk from being uninephric postoperatively. Infectious disease and malignancy clearance are also required. Finally, renal imaging to compare the size of the kidneys and their vasculature was performed to determine the laterality of the donor procedure..
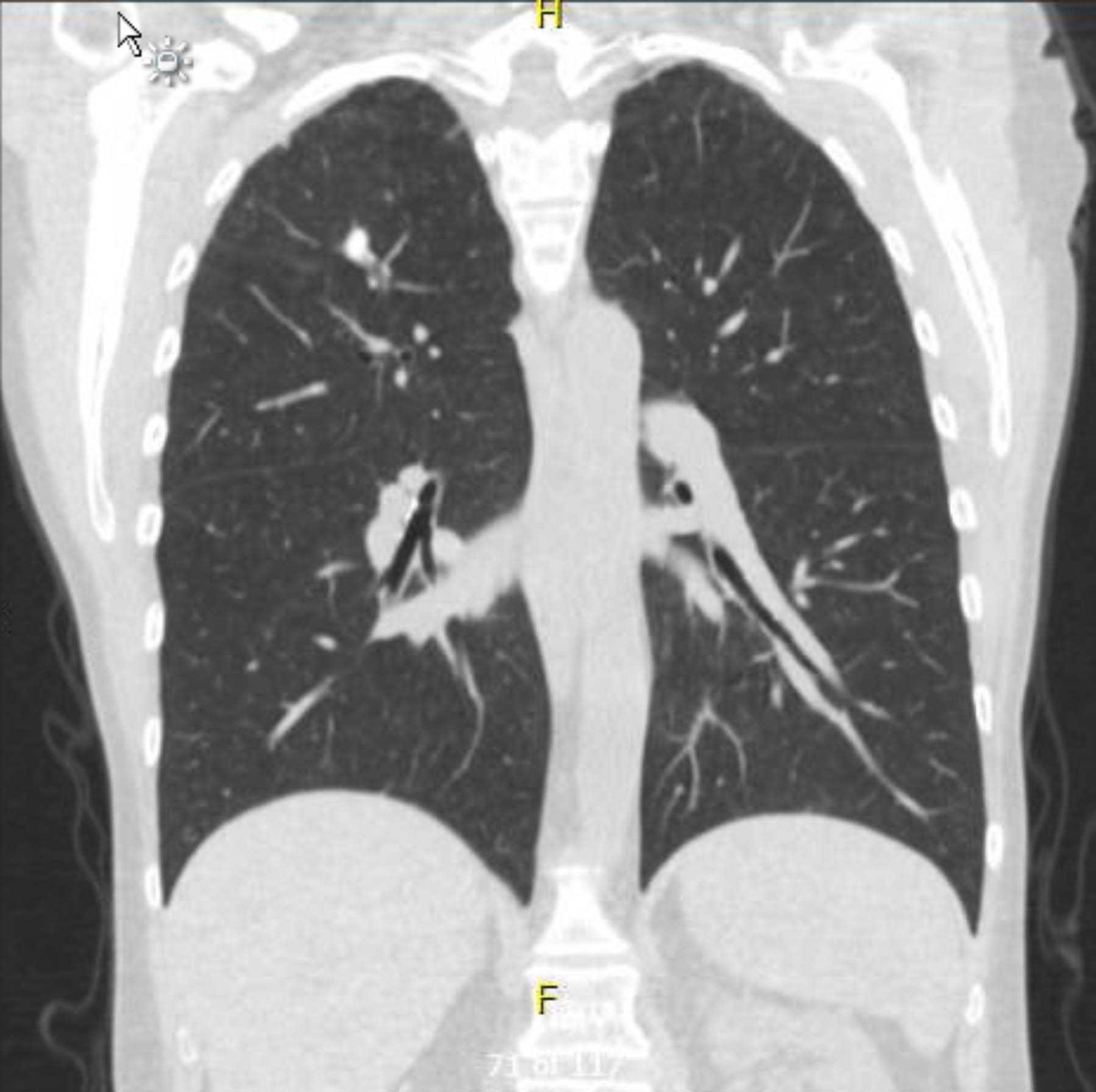
Figure 1. Preoperative Non-contrast Chest CT. Coronal View. Granulomatous changes in the right apex.
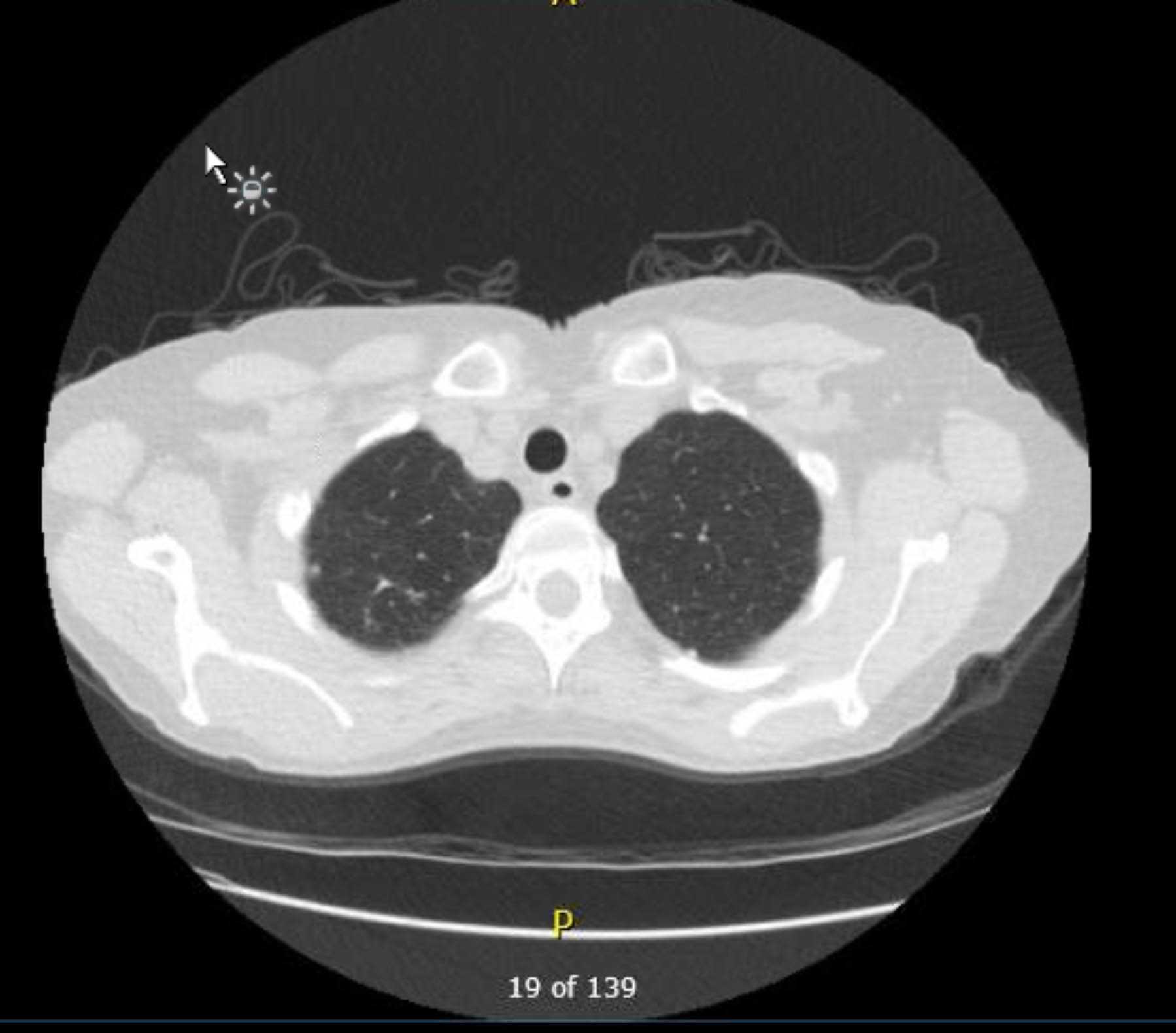
Figure 2. Preoperative Non-contrast Chest CT. Axial View. Granulomatous changes in the right apex.
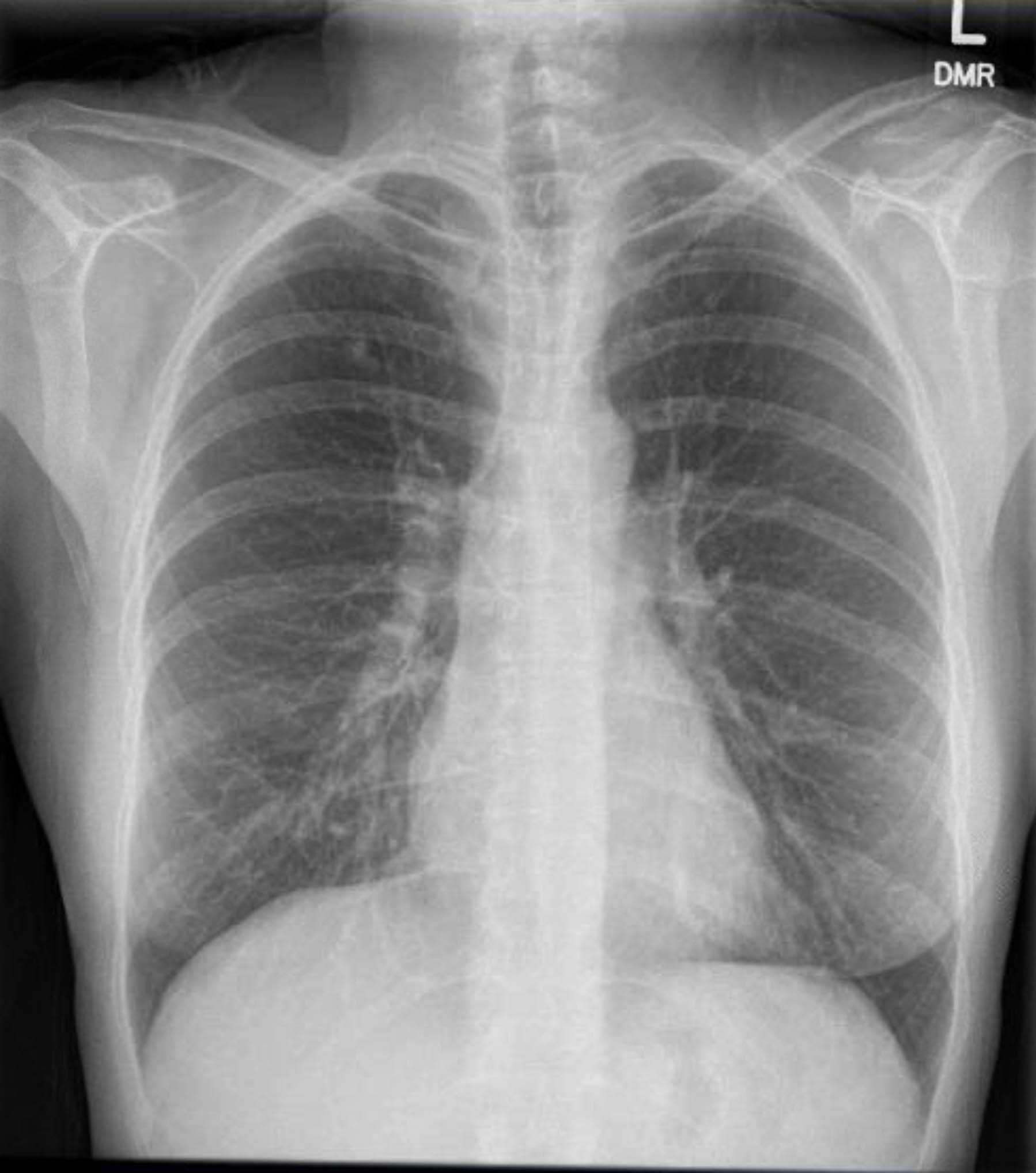
Figure 3. Preoperative Chest X-ray. Calcified granulomas in the right upper lobe.
Natural History
ESRD has a very heterogeneous presentation and disease progression. In the United States, the most common cause of chronic renal failure is diabetes mellitus, which accounts for 45% of all renal failure. The second and third most common causes are hypertensive nephropathy (27%) and chronic glomerulonephritis (11%), respectively.4 Progression of CKD to ESRD requires a patient to undergo hemodialysis to aid in whole body fluid balance and filtration of electrolytes, metabolites, hormones, and toxins. If the patient does not undergo dialysis, they must undergo kidney transplantation or their disease will be fatal.
Options for Treatment
The treatment options for ESRD are dialysis (peritoneal dialysis or hemodialysis) and/or transplantation. In the United States in 2018, 85.9% of all incident cases of ESRD began renal replacement therapy with hemodialysis, 10.9% started with peritoneal dialysis, and 2.9% received a preemptive kidney transplant.5
Kidney transplantation occurs from either a deceased or a living donor. If a family member or friend wishes to donate but is incompatible, live-donor paired exchange (where a donor exchanges their donation with another donor so the recipients receive compatible kidneys) could be an option, which would exchange donors who are incompatible with their intended recipients so that instead each donor donates a kidney to a compatible recipient. Finally, non-directed altruistic donors require a very rigorous process to carefully select a donor and in one study it was found that almost 60 percent of non-directed altruistic donors dropped out after initial evaluation and education session, thus making this a non-sustainable source of donors.6 If the altruistic donors complete the evaluation and are accepted as potential donor candidates, it is our practice to have them start a paired exchange chain. This is done by matching them with a recipient who has an incompatible donor, who will then donate to someone else, and so forth. Multiple recipients will benefit as opposed to matching them with one recipient.
Rationale for Treatment
Despite a variety of treatment modalities for ESRD, kidney transplantation remains the most definitive and durable renal replacement therapy. It offers an improved quality of life, is more cost-effective than dialysis, and has an overall improved survival.3 In fact, life expectancy approximately doubles with kidney transplant across all age ranges when comparing mortality of pretransplant patients to post-transplant patients.4
When choosing between a deceased and living donor kidney, several studies have determined that living donor kidneys have better post-transplant outcomes with lower incidences of delayed graft function postoperatively given the short ischemic time. Living donors also provide longer kidney graft functions in the recipient, likely related to the donor being healthy. Other benefits include avoidance of prolonged waiting time on dialysis and the ability to coordinate donor and recipient procedures in a timely fashion.3 The best postoperative graft survival has been found in patients that receive kidney transplantation predialysis initiation.4 For the patient presented here, she was able to find a living related donor prior to initiating hemodialysis thus has the highest likelihood of graft survival when compared to patients who receive a deceased donor kidney or transplantation after being on dialysis.
Special Considerations
As mentioned above, given the variable presentation of ESRD and differences in progression of disease, a very thorough preoperative evaluation with complete history, physical exam, and appropriate imaging is necessary. The absolute contraindications to kidney transplant that need to be ruled out preoperatively include active infection, malignancy, active substance abuse, and poorly controlled psychiatric illness.3 Other important considerations include a thorough cardiovascular and peripheral vascular evaluation as these both could preclude the patient from being a suitable kidney recipient.
Discussion
Emerich Ullman reported the first attempt at kidney transplantation in 1902, but the first successful kidney transplant was not completed until 1954 when Joseph Murray circumvented the immunologic barrier and completed a kidney transplant between two identical twins without using any immunosuppression.3 In the same decade, steroids and radiation were the first immunosuppressants used, but it was the introduction of Azathioprine (Imuran) around 1960 that began a new era of kidney transplantation. Throughout the next three decades, immunosuppression continued to evolve such that these medications now have a lower toxicity profile and are better tolerated by patients.7
Unfortunately, the biggest challenge to transplantation is the shortage of organs available for those in need. The success of solid organ transplantation is ironically the single factor most responsible for the critical shortage; improved survival rates and tolerance of immunosuppression has encouraged both physicians and patients to opt for transplantation.1,8 Patients in need of these organs are those that suffer from ESRD. In 2018, the prevalence of ESRD in the United States was 785,883 with an incidence of 131,779.5 There are 88,627 people on the kidney transplant waitlist with approximately 3,700 patients being added each month. The number of kidney transplants performed yearly from both living and deceased kidney donors has increased, but it remains less than 30,000 (25,500 in 2022).9 Thus the median wait time is 3.6 years.10 The patient presented in this case is a 56-year-old female who suffered from ESRD secondary to diabetic and hypertensive nephropathies and underwent a preemptive living related kidney transplant.
Preemptive kidney transplant is a unique situation in that the patient with ESRD has not yet initiated dialysis before undergoing transplantation. Only 2.9% of patients in the US underwent kidney transplantation as their initial mode of ESRD therapy.5 In review of the literature, there are several papers that suggest that living donation provides better patient and allograft survival when compared with deceased-donor transplantation, especially when the live donor transplant is performed preemptively without dialysis.6 Living donor transplantation reduces wait times on dialysis, has shorter and less expensive hospital stays, and overall improved post-transplant outcomes.11 When done prior to dialysis initiation, the patient is able to avoid the morbidity of dialysis, dialysis access procedures, and the cost associated with this treatment. Waiting time on dialysis before transplantation has been studied and shown to quantitatively be one of the largest independent risk factors for graft loss after kidney transplant.12 Postoperative outcomes of patients that receive a transplant predialysis show lower rates of delayed graft function when compared to non-preemptive transplants.13 From a donor perspective, the living kidney donors have survival similar to that of non-donors, and their risk of ESRD is not significantly increased.14
From a surgical perspective, there were several decisions made throughout this case that warrant further discussion. The first clinical decision was related to the surgical exposure. In the history of kidney transplant, there was a time when the upper thigh was the location of transplantation. However, this was discontinued because it requires a skin ureterostomy, which is at significantly higher risk for ascending infection. In 1956, Merrill and Murray described the first transplant using the iliac fossa. They noted that the renal fossa was not chosen because it requires simultaneous nephrectomy and necessitates an ureteroureteral anastomosis, which places the ureter at high risk of stricture formation. As a result, it was concluded that the iliac fossa allowed access to adequate blood supply using the iliac vessels as well as an accessible ureteral drainage into the bladder directly via ureteroneocystostomy.15 Kidneys are typically placed in the right iliac fossa (the contralateral side of donated kidney) because most donor nephrectomies are left sided given the increased length of the renal vein.2 However, in this case presentation, the patient underwent transplantation into the left iliac fossa given that she has a history of type I diabetes mellitus and may require a pancreas transplant in the future (which are usually placed in the right iliac fossa). The last approach that is sometimes considered, pending the patient’s prior surgical history and vascular anatomy, is an intraperitoneal approach.
The next significant step in this operation is the vascular anastomoses. The renal vein is most often anastomosed first and usually to the external iliac vein in an end-to-side fashion, but this location varies relative to the arterial anastomosis. The arterial anastomosis can connect the donor renal artery with the recipient common, external, or internal iliac artery, and the procedure has evolved over time. Historically, the internal iliac was preferentially selected for an end-to-end anastomosis to the donor renal artery; however, this was not shown to be superior to the later approach of end-to-side of the renal artery to the common or external iliac artery. Thus, the most common anastomosis performed today is between donor renal artery and the side of the recipient external iliac artery as this vessel has no branches in the pelvis and is in close proximity to the bladder which facilitates the creation of the ureteroneocystostomy without compromising the distal ureteric blood supply. If the kidney was recovered from a deceased donor, the donor aorta is also recovered and could be fashioned into a Carrel patch and used for the anastomosis to the common or external iliac artery.2 During the procurement of the donor kidney, one important consideration is the number of renal arteries. When the donor is a deceased donor, it is possible to preserve all renal arteries originating from the donor aorta, including their origins in the Carrel patch. However, in a living donor, this is not feasible and multiple arteries are either anastomosed separately, or more commonly, they are anastomosed together into one artery prior to implanting the kidney. If there are small accessory arteries supplying the upper pole of the kidney, they are often ligated. Lower pole arteries are more likely to supply the ureter and consequently less likely to be ligated as the blood supply to the ureter needs to be optimal.
The final anastomosis to consider is the construction of the donor ureteral to recipient bladder anastomosis. Throughout the years of kidney transplantation there have been several approaches to the ureteroneocystostomy, the implantation of the donor ureter into the recipient bladder. Initially, the most widely used anastomosis was the Leadbetter-Politano technique, an intravesical technique that requires exposure via an anterior cystostomy to allow submucosal tunneling of the ureter and placement of the neo-orifice in a near anatomic location.16 The more recent extravesical approach, developed by Lich and Gregoir, is employed by most transplant centers today and is the approach used in this case. A single small cystotomy is created at the bladder dome, and the distal donor ureter is anastomosed to the bladder mucosa. A seromuscluar layer is then closed over the ureter.2 The final method is an ureteropyelostomy, an anastomosis between the recipient ureter to the lowest portion of the donor renal pelvis. This approach is not frequently used because it often requires an ipsilateral native nephrectomy and has been shown to have a higher ureteral leak rate.2
The final consideration in this case - and one that remains controversial in the kidney transplant literature - is the use of a ureteral stent. Several studies have investigated the risks and benefits of ureteral stents. Of the urological complications after renal transplantation, most originate from the vesicoureteric anastomosis. The therapeutic benefit of a ureteral stent is that it simplifies the creation of a watertight ureteric mucosa to bladder mucosa anastomosis and reduces anatomic kinking. However, the significant risks associated with the use of a stent include recurrent urinary tract infections and eventual graft loss. Overall, the literature has not been able to adequately assess the morbidity and cost of universal stenting, and therefore, this practice remains a surgeon-to-surgeon assessment and decision at the time of surgery.17 In this case, the attending surgeon discovered that the donor kidney had an extra renal pelvis, and prior to completing the ureteral anastomosis, there appeared to be a fullness of the renal pelvis. Consequently, a 4.7 Fr. double J stent was placed.
In summary, this case highlights a living related preemptive kidney transplant. The patient presented was fortunate enough to have a living donor who was not only willing to donate but was deemed suitable for donation as well. The outcomes of living donation are superior to deceased donation, especially when performed prior to the initiation of dialysis, as was the case with this patient. As the wait list for kidney transplantation continues to grow, the importance of living donation will continue to increase. It is therefore imperative for kidney transplant centers throughout the United States to encourage living donation. One promising development is the dissemination of laparoscopic donor nephrectomies. This technique, now used in more than 90% of donor nephrectomies, reduces the recovery time for living donors.11 This is one example of the work that needs to continue to incentivize donation - both decreased and living - in order to help combat the shortage of organs for those with ESRD.
Equipment
Fogarty Hydragrip Clamps were used when clamping the iliac vessels. Edward Lifesciences provides the Hydragrip inserts for the Fogarty Clamp. These less traumatic clamps are believed to decrease the risk of dissection. When performing the arterial anastomosis, an aortic punch by Teleflex Medical is used for the arteriotomy.
Disclosures
None.
Acknowledgements
Corey Eymard, MGH Transplant Fellow performed this procedure with Dr. Nahel Elias.
Statement of Consent
Consent for the use of clinical history, radiology, and intraoperative video was obtained from the patient and providers involved in compilation of this case report and filming.
Citations
- Institute for Healthcare Improvement. Organ Donation Update: Success Brings New Challenges. Available at: http://www.ihi.org/resources/Pages/ImprovementStories/OrganDonationUpdateSuccessBringsNewChallenges.aspx
- Pereira BJG, Sayegh MH, Blake P. Chronic Kidney Disease, Dialysis, & Transplantation. 2nd ed. Philadelphia, PA: Elsevier Saunders; 2005.
- Humar A, Dunn DL. Chapter 11: Transplantation. In: Schwartz’s Principles of Surgery. 9e ed. New York, NY: McGraw-Hill; 2010.
- Punch, JD. Chapter 45: Organ Transplantation. In: Current Diagnosis & Treatment. 13e ed. 16,New York, NY: McGraw-Hill; 2006.16. Monga M. Ureteroscopy. New York: Humana Press, 2013.
- United States Renal Data System. 2020 USRDS Annual Data Report: Epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2020.
- Davis CL, Delmonico FL. Living-donor kidney transplantation: a review of the current practices for the live donor. J Am Soc Nephrol. 2005 Jul;16(7):2098-110. doi:10.1681/ASN.2004100824.
- Murray JE, Merrill JP, Harrison JH, Wilson RE, Dammin GJ. Prolonged survival of human-kidney homografts by immunosuppressive drug therapy. N Engl J Med. 1963 Jun 13;268:1315-23. doi:10.1056/NEJM196306132682401.
- Klein AS, Messersmith EE, Ratner LE, Kochik R, Baliga PK, Ojo AO. Organ donation and utilization in the United States, 1999-2008. Am J Transplant. 2010 Apr;10(4 Pt 2):973-86. doi:10.1111/j.1600-6143.2009.03008.x.
- Organ Procurement and Transplantation Network. Data. Available at: https://optn.transplant.hrsa.gov/data.
- Organ Donation and Transplantation Statistics. National Kidney Foundation. 2016. Available at: https://www.kidney.org/news/newsroom/factsheets/Organ-Donation-and-Transplantation-Stats.
- Axelrod DA, McCullough KP, Brewer ED, Becker BN, Segev DL, Rao PS. Kidney and pancreas transplantation in the United States, 1999-2008: the changing face of living donation. Am J Transplant. 2010 Apr;10(4 Pt 2):987-1002. doi:10.1111/j.1600-6143.2010.03022.x.
- Meier-Kriesche HU, Kaplan B. Waiting time on dialysis as the strongest modifiable risk factor for renal transplant outcomes: a paired donor kidney analysis. Transplantation. 2002 Nov 27;74(10):1377-81. doi:10.1097/00007890-200211270-00005.
- Kasiske BL, Snyder JJ, Matas AJ, Ellison MD, Gill JS, Kausz AT. Preemptive kidney transplantation: the advantage and the advantaged. J Am Soc Nephrol. 2002 May;13(5):1358-64. doi:10.1097/01.asn.0000013295.11876.c9.
- Ibrahim HN, Foley R, Tan L, et al. Long-term consequences of kidney donation. N Engl J Med. 2009 Jan 29;360(5):459-69. doi:10.1056/NEJMoa0804883.
- Merrill JP, Murray JE, Harrison JH, Guild WR. Successful homotransplantation of the human kidney between identical twins. J Am Med Assoc. 1956 Jan 28;160(4):277-82. doi:10.1001/jama.1956.02960390027008.
- Monga M. Ureteroscopy. New York: Humana Press, 2013.
- Wilson CH, Bhatti AA, Rix DA, Manas DM. Routine intraoperative stenting for renal transplant recipients. Transplantation. 2005 Oct 15;80(7):877-82. doi:10.1097/01.tp.0000181197.21706.fa.
- Aravindan N, Shaw A. Effect of furosemide infusion on renal hemodynamics and angiogenesis gene expression in acute renal ischemia/reperfusion. Ren Fail. 2006;28(1):25-35. doi:10.1080/08860220500461229.
- Siedlecki A, Irish W, Brennan DC. Delayed graft function in the kidney transplant. Am J Transplant. 2011 Nov;11(11):2279-96. doi:10.1111/j.1600-6143.2011.03754.x.

