Laser Stapedotomy for Otosclerosis
Abstract
Otosclerosis can lead to progressive conductive hearing loss, significantly affecting quality of life. For patients who choose surgery, the tympanic membrane is elevated, and the middle ear space is explored. If the surgeon confirms that the stapes is fixed in the oval window, either a stapedotomy or stapedectomy can be performed. In the stapedotomy, the surgeon removes the stapes superstructure, creates a fenestration in the footplate, and places a prosthesis from the incus through the fenestration into the vestibule. In this instance, the patient was able to regain nearly all of the hearing that had been lost as a result of stapes fixation.
Case Overview
Clinical Presentation
Typical for most patients with otosclerosis, our patient presented with gradually progressive hearing loss over many years. The patient denied any significant otologic history such as ear surgery, ear infections, trauma, noise exposure, or ototoxic medications. The patient’s mother had hearing loss in her late 40s and used a hearing aid.
Physical Exam
On physical exam, the patient’s external ears were normal in appearance. The external auditory canals were normal. The tympanic membranes were clear, without retraction or evidence of inflammation or middle ear effusion. There was no evidence of “Schwartze sign”, a pink coloration of the promontory suggestive of active otosclerosis. A tuning fork exam (512 Hz) was performed, demonstrating bone conduction greater than air conduction in the left ear (negative Rinne). A Weber test was performed, with lateralization to the left ear, confirming a conductive hearing loss. At 512 Hz, this is indicative of at least a 25-dB air-bone-gap. Negative Rinne tests at 256 Hz and 1024 Hz imply air-bone-gap levels of 15 dB and 35 dB, respectively.
Adjunctive Studies
The patient’s audiogram demonstrated a conductive hearing loss across all frequencies. Hearing loss typically begins in the lower frequencies and advances to involve higher frequencies as the fixation becomes more widespread.
There was a “Carhart notch” at the 2000-Hz frequency (Figure 1). This is a mechanical artifact of testing, not a true sensorineural hearing loss. The normal ossicular resonance in humans is around 2000 Hz, which is impaired by stapes fixation.
Acoustic reflexes are also an important component of workup. If the stapes is affected by otosclerosis, corresponding reflexes will be decreased or absent in the affected ear. Tympanometry may also show a decreased (As) peak due to reduced compliance.
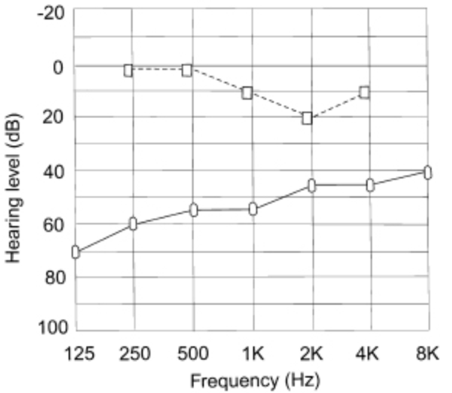
Figure 1. Typical audiogram of a patient with otosclerosis. The Carhart effect is demonstrated at 2000 Hz.
Natural History
The majority of patients experience noticeable hearing loss in the 4th decade of life but may present with symptoms before or after this time. Given the heterogeneity of the disease process, predicting the progression and endpoint of the hearing loss remains difficult, particularly in instances of cochlear otosclerosis.
Options for Treatment
Patients can elect to observe their hearing loss, amplify environmental sounds with hearing aids, or undergo surgical intervention. Patients with poor speech discrimination scores preoperatively are likely to benefit less from surgery and should be counseled as such.
Rationale for Treatment
In this case, the patient’s hearing loss was significantly impacting her quality of life. She did not want to wear hearing aids and elected to undergo surgery.
Special Considerations
Patients with active middle ear infections or tympanic membrane perforations should not have a stapedotomy.
Step-by-Step Technique
Anesthesia
Stapedotomy can be performed under general or local anesthesia. This can be determined based on the patient’s health status as well as patient preference. Performance of stapedotomy under local anesthesia provides the advantage of detecting the onset of any vestibular symptoms.
Patient Positioning
The patient is placed in the supine position with the head turned away from the operative side. The bed is rotated 180 degrees to allow the surgeon and assistant to work unencumbered by the anesthesiology setup.
Facial Nerve Monitoring
Given the proximity of the facial nerve to the oval window, the authors perform stapedotomy procedures with bimodal facial nerve monitoring electrodes, placed into the ipsilateral orbicularis oculi and oris muscles.
Prepping the Patient
The ear canal, ear, and a space around 10 cm beyond the auricle are prepped with Betadine solution. The patient is then draped in standard fashion. An injection of local anesthetic with epinephrine can be performed under the microscope prior to prepping the patient to allow for more time to elapse prior to starting the procedure.
Procedure Details
After prepping and draping the ear, the canal is examined under the operative microscope. The canal is irrigated of the prep solution with care not to injure the skin of the external auditory canal. There are multiple incisions that can be used for the tympanomeatal flap.
- Type 1: A curvilinear incision is made starting 3 mm lateral to the annulus at the 6 o’clock position. This is curved posteriorly to a distance of approximately 7 mm lateral to the annulus and then extending superiorly to the 12 o’clock position approximately 4 mm lateral to the annulus.
- Type 2: A straight incision is made from the 6 o’clock position from the annulus to 6–7 mm laterally. A second straight incision is made from the 12 o’clock position from the annulus to a similar distance laterally, and the two incisions are then connected. </p>
Regardless of the method for the tympanomeatal flap, there is a balance of “too short” versus “too long”. If the flap is too long, it becomes obstructive and inhibits the anterior visualization. If it is too short, then it may not cover the middle ear space after the scutum has been removed.
The tympanomeatal flap is elevated medially with care not to tear the flap. When the annulus is reached, it is elevated from the sulcus in the posteroinferior quadrant. It is elevated inferiorly to the 6 o’clock position. There are several small vessels in this area, and a piece of gelfoam with epinephrine may be applied for hemostasis as well as to keep the flap elevated. The annulus is elevated superiorly, and the chorda tympani nerve is identified. This should be atraumatically separated from the annulus and tympanic membrane, avoiding stretching the nerve as this can result in dysgeusia. The ossicular chain should be palpated to rule out fixation of the malleus or the incus, and to confirm fixation of the stapes. Typically, stapes fixation will result in a hypermobile incudostapedial (IS) joint. The round window should also be examined to ensure that obliteration has not occurred.
Typically, the scutum must be removed to provide visualization and access to the IS joint and the stapes/oval window. This can be accomplished with either the curette or the drill. Next, the IS joint is separated. This should be done in a posterior-to-anterior direction, allowing for the stapedial tendon to provide counter-traction during separation. When separated, the tendon can be divided sharply or with the laser. The posterior crus of the stapes is then divided with the laser usually near the footplate to prevent a long remnant, which could scar to the prosthesis. The stapes is carefully downfractured with a rosen needle, and the stapes is removed. With the footplate in view, the distance from the footplate to the long process of the incus is measured to determine the appropriate prosthesis length. Next, we create a rosette pattern using the laser at a setting of 500 mW. This allows either the 0.7-mm drill or serial dilation with hand drills to open the footplate and oval window. We position this at the junction of the posterior 1/3 and anterior 2/3 of the footplate to reduce the likelihood of injury to the vestibular organs. The prosthesis is then placed over the incus and within the stapedotomy. Palpation of the ossicular chain should confirm movement of the prosthesis within the stapedotomy. In some instances, a small amount of irrigation can be placed in the round window niche, and a reflex can be observed. A blood patch or a small amount of soft tissue can be placed around the distal end of the prosthesis. The tympanomeatal flap is returned to its position.
Closure
The tympanomeatal flap is laid back into place, ensuring that the annulus sits in the groove. Either a thin layer of ointment, or several small strips of Gelfoam with Ciprodex solution can be placed over the incision lines.
Dressing
A cotton ball and Band-Aid are placed on the outer ear. A Glasscock/mastoid dressing are not necessary.
Postoperative Restrictions
The ear may be filled (partially or completely) with either ointment or Gelfoam at surgery, requiring time to dissolve or to be removed. Typically, drops (ofloxacin 0.3% otic solution, Ciprodex 0.3%/0.1% otic solution) are prescribed, and patients are instructed to apply 3–5 drops once or twice a day for 1–3 weeks. Patients should not allow water to enter the ear for at least 4 weeks after surgery until full healing has been confirmed at a follow-up appointment. This is accomplished by coating a cotton ball with Vaseline and placing it in the meatus when showering. They should not submerge in either a bath or pool during this time. Patients should also avoid significant straining or restrictive sneezing/coughing. A stool softener can aid in bowel movements, and should the patient need to sneeze or cough, he should do so with his mouth open rather than stifling it. Follow-up typically occurs at 3–4 weeks to ensure that everything is healing and that there is no infection. An audiogram is then performed 3 months postoperatively. If a patient experiences any significant vertigo or nausea postoperatively, they can be given aggressive antiemetics (Phenergan PR is quite effective). If vertigo is disabling, a short course of steroids can be prescribed. This typically resolves in 24–48 hours.
Equipment
- Standard microscopic ear tray instruments.
- Laser: The selection of laser type is dependent on both surgeon and institutional preferences. The carbon dioxide or iridium lasers are both effective.
- Drill: If the footplate or scutum requires drilling, this can be accomplished with small caliber drills (0.6–0.8 mm) set to lower RPM (8,000–10,000).
- Prosthesis: A wide variety of prostheses are available for use, typically dictated by surgeon preference.
Disclosure
Author C. Scott Brown also works as editor of the Otolaryngology section of the Journal of Medical Insight.
Statement of Consent
The patient referred to in this video article has given their informed consent to be filmed and is aware that information and images will be published online.
Citations
- De Souza CE, Kirtane MV. Otosclerosis. Otorhinolaryngology – Head and Neck Surgery Series Otology and Neurotology. Noida, Uttar Pradesh, India: Thieme; 2013:204-226.
- Harrell RW. Pure tone evaluation. Handbook of Clinical Audiology. 5th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2001:71-87.