Open Left Colectomy for Colon Cancer: Left Colon and Sigmoid Resection with Colostomy Formation
Abstract
An open colectomy is the resection of all or part of the colon, typically through a midline incision in the abdomen. This procedure is often indicated for the treatment of colonic diseases such as bowel obstruction, diverticulitis, inflammatory bowel disease, and colon cancer. The patient in this case was a C6 quadriplegic male who presented with colon cancer near the splenic flexure. He also suffered from colonic dysmotility and severe constipation. He was treated with an open left colectomy through an upper midline laparotomy. Regarding the procedure, once the abdomen was entered, the peritoneal cavity was explored, and the tumor was identified. The colon was mobilized, starting with the transverse colon, which was extended laterally to take down the hepatic flexure followed by mobilization of the right colon in a lateral-to-medial fashion. Next, the splenic flexure was mobilized followed by the descending colon, again in a lateral-to-medial fashion. Once mobilized, the margins of transection were identified, and the intervening mesocolon was ligated in a cut and tie fashion. The colon was then transected using and ILA stapler to include the distal transverse, descending, and proximal sigmoid colon. Finally, the proximal cut end of the transverse colon was brought up through a left-sided end colostomy. In this video, the key steps of the procedure are demonstrated, and we provide analysis regarding our intraoperative decision making.
Case Overview
Background
Colon cancer is a malignant process involving the epithelial lining of the colon. It is the third most common cancer in the world, accounting for approximately 9% of new cancer diagnoses.1 The incidence of colon cancer is geographically variable, suggesting that both genetic and lifestyle factors contribute to the development of disease. Western Africa has the lowest incidence, with a rate of 3–4 cases per 100,000 persons per year, whereas North America has an annual incidence of 26 per 100,000 persons.2 In addition, colon cancer represents the fourth most common cause of cancer-related death with over 700,000 cases annually.3 Taken together, this condition represents a major global health issue for both developed and developing nations.
Risk factors for colon cancer include age, environmental factors, and genetic predisposition. The median age of diagnosis is 67 years for men and 71 years for women.4 While the advent of regular screening colonoscopy has helped to reduce the incidence of colon cancers in patients greater than 50 years old, there has been a doubling in the incidence of colon cancer amongst younger patients, primarily aged 40–49, over the last several decades.5 The rise in incidence in younger populations is likely associated with increasing rates of obesity, sedentary lifestyle, Western diet, metabolic syndrome, as well as alcohol and tobacco use. These observations have been similarly observed in other industrialized countries. Finally, familial studies indicate that up to 30% of colon cancers are related to an inherited form of disease, and approximately 5% of cases are linked to highly penetrant colorectal cancer syndromes including familial adenomatous polyposis (FAP), Lynch syndrome, and hamartomatous conditions.6
Surgical resection remains the only curative therapy for colon cancer. Once a diagnosis is established, most commonly through screening colonscopy, patients are fully staged using the American Joint Committee on Cancer (AJCC) TNM system. For patients with localized or regional disease, colectomy with a yield of at least 12 lymph nodes is the standard of care. Adjuvant chemotherapy is considered for patients with high risk features or positive node status. Finally, for patients presenting with metastatic disease, the majority of these cases are considered incurable and patients are treated with palliative chemotherapy. Survival for colon cancer has significantly improved with better surgical techniques and chemotherapy regimens. The average 5-year survival rate for early stage disease is greater than 90%; involvement of lymph nodes reduces this to approximately 70%, and metastatic disease is still associated with a dismal prognosis with less than 15% of patients surviving beyond 5 years.7
In this video, we perform an open left colectomy on a 65-year-old patient who presented with a large bowel obstruction secondary to tumor. In this procedure, the colon is mobilized bilaterally, including takedown of both the hepatic and splenic flexures. The distal transverse, descending, and proximal sigmoid colon are resected and an end colostomy is created. Therefore, this procedure adequately resects the diseased portion of the colon, effectively treating this condition.
Focused History of the Patient
The patient is a 65-year-old male with quadriplegia after a traumatic C6 cord injury who presented to an outside hospital with new onset nausea, vomiting, and obstipation. His workup included an abdominal CT scan with evidence of an obstructing mass in the transverse colon. He was clinically stable and was transferred to the Massachusetts General Hospital for further care. His medical history is notable for chronic constipation, recurrent decubitus ulcers treated with multiple operations, including a Girdlestone procedure, and recurrent pyelonephritis secondary to kidney stones status post lithotripsy and left-sided percutaneous nephrostomy tube placement. He has an American Society of Anesthesiologist score (ASA) of 3 and his body mass index (BMI) is 25. Given that he was obstructed, the patient was taken directly to the operating room for definitive treatment.
Physical Exam
The patient had an unremarkable physical exam. In the office, he presented in a wheelchair and was in no apparent distress with normal vitals. He had a normal habitus. His abdominal exam was significant for prior surgical scars, no evidence of hernias, and no tenderness to palpation. His abdomen was distended but soft.
Imaging
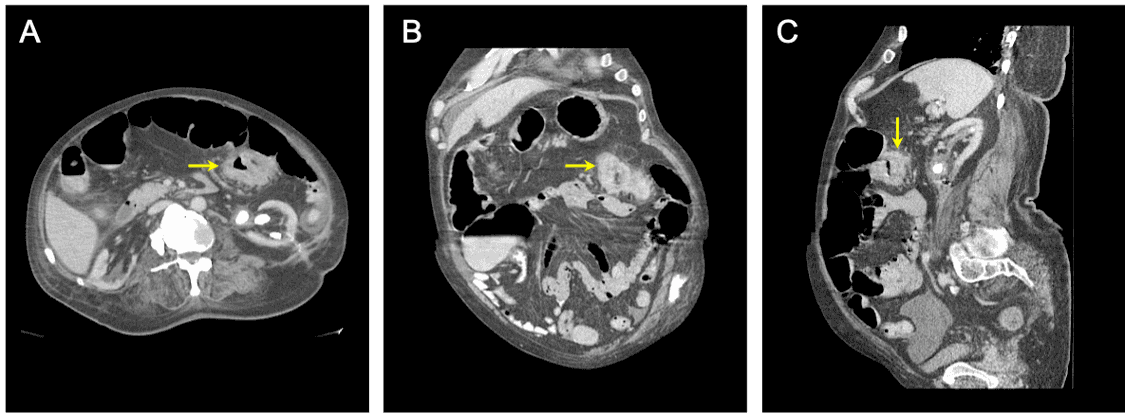
Figure 1: Abdominal and pelvic CT scans. CT scan of the abdomen and pelvis with intravenous and oral contrast showing evidence of an obstructing transverse colon mass. The diseased tissue is shown in (A) axial, (B) coronal, and (C) sagittal views. Yellow arrows point towards the diseased segment of the colon.
Natural History
Multiple pathogenic mechanisms have been implicated in the development of colon cancer. For the majority of patients, a stepwise sequence of genetic and epigenetic alterations in colonic epithelia leads to development of benign polyp neoplasms that can progress to invasive carcinoma over a period of years, as initially described by Vogelstein et al.8 Genetic alterations have been shown to occur in three main mechanisms, including chromosomal instability, microsatellite instability, and CpG island methylation.9 In addition, a subset of patients may develop colon cancer secondary to significant chronic inflammation that can incur dysplastic changes without polyp formation, typically in individuals with ulcerative colitis or Crohn’s colitis. Similarly, individuals with Lynch syndrome, a germline condition resulting in microsatellite instability, will develop colon cancers without polyp formation. Once an invasive cancer has developed, malignant cells invade and disrupt surrounding tissues and can spread to distant sites via lymphatic, perineural, and hematogenous invasion.
Options for Treatment
For patients with localized, regional metastatic, or certain instances of oligometastatic colon cancer, surgical resection remains the only potential curative therapy. Nonetheless, the patient should discuss the risks and benefits of an operation with their surgeon. Adjuvant chemotherapy is frequently indicated for disease with aggressive features or disease that has spread to lymph nodes or distant organ sites. However, chemotherapy alone cannot cure this condition.
Rationale for Treatment
In general, the goal of surgical resection is complete extirpation of malignant tissue, thus a curative intent.
Special Considerations
There can be certain instances in which the cancer has spread to distant sites though a complication with the primary tumor has occurred, including significant bleeding, perforation, or obstruction. In these situations, a surgeon may decide to operate as an acute life-saving intervention without a goal of disease clearance. In this video, the patient presented with a complication, a large bowel obstruction, but fortunately did not have evidence of metastatic disease.
Discussion
As we have shown in this video, the main procedural steps for this operation are as follows: (1) perform midline laparotomy and survey the peritoneal cavity, (2) mobilize the transverse colon via take-down of the gastrocolic ligament and entry into the lesser sac, (3) hepatic flexure takedown and lateral-to-medial mobilization of the ascending colon, (4) splenic flexure takedown and lateral-to-medial mobilization of the descending and sigmoid colon, (5) identify margins of resection and ligate intervening mesocolon, (6) transect the colon using an ILA 100 stapler, and (7) create an end colostomy in a brooked fashion. This approach to an open colectomy results in extensive mobilization of the entire colon, allowing a large resection and a subsequent tension-free end colostomy on the left-side of the abdomen. The middle colic artery is preserved, ensuring adequate blood supply to the remaining, distal transverse colon.
For colon cancer surgery, the extent of nodal yield and mesocolic excision remains an area of open debate. Le Voyer et al. previously showed that the number of lymph nodes analyzed in colon cancer specimens was associated with survival.10 Consequently, current guidelines recommend that a minimum of 12 lymph nodes be resected with the cancer specimen for adequate staging. The reason for why a higher nodal yield is linked to better survival outcomes is not fully understood. Stage migration, in which cancers are upstaged with higher nodal yields as the likelihood of finding a positive node increases, is thought to contribute to a certain extent.11 However, it has also been proposed that a more extensive mesocolic excision provides a more adequate extirpation of regional micrometastatic disease.12 In support of this reasoning, multiple studies have shown that extensive mesocolic excision is associated with improved disease-free and overall survival rates amongst colon cancer patients.13, 14 In this video, the mesocolon was taken close to the vascular takeoffs to provide a larger mesocolic specimen.
Going forward, there will continue to be improvements in non-surgical treatments for colon cancer. With improved rates of screening colonoscopy, earlier detection and endoscopic polypectomy have been shown to be sufficient for the treatment of very early cancers, obviating the need for an operation in a subset of individuals.15 Systemic therapies have also undergone significant evolution and improvement. Newly designed targeted therapies against vascular endothelial growth factor (VEGF), epidermal growth factor receptor (EGFR), and components of the KRAS pathway might have added benefit to current chemotherapy regimens and are undergoing clinical investigation.16, 17 Finally, the recent development of immunotherapy might have promise for the subset of colon cancers defined by microsatellite instability.18
Patient Outcome Statistics from Procedure
- Operative time: 90 minutes
- Estimated blood loss: 400 mL
- Fluids: 4600 mL crystalloid
- Length of stay: discharged from hospital to home with visiting nursing assistance on postoperative day 9
- Morbidity: no complications
- Final pathology: pT4aN2bM0, 8 of 17 positive nodes; histology: poorly differentiated with lymphovascular invasion, surgical margins all negative
Equipment
- 10-blade scalpel
- Electrocautery
- DeBakey forceps
- Abdominal wall handheld retractor
- Schnidt clamp
- 3-0 and 2-0 silk ties for ligation of mesentery
- Metzenbaum scissors
- 100-mm blue load ILA stapler
- 4-0 Vicryl for maturing colostomy
- 1-0 Prolene suture for fascial closure
- Skin stapler
Disclosures
Nothing to disclose.
Statement of Consent
The patient referred to in this video article has given their informed consent to be filmed and is aware that information and images will be published online.
Acknowledgments
We would like to thank Theresa Kim, MD for assisting in this operation.
Citations
- Mattiuzzi C, Sanchis-Gomar F, Lippi G. Concise update on colorectal cancer epidemiology. Ann Transl Med. 2019;7:609. doi:10.21037/atm.2019.07.91.
- Kuipers EJ, Grady WM, Lieberman D, et al. Colorectal cancer. Nat Rev Dis Primers. 2015;1:15065. doi:10.1038/nrdp.2015.65.
- Mortality GBD, Causes of Death C. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385:117-71. doi:10.1016/S0140-6736(14)61682-2.
- Siegel R, Desantis C, Jemal A. Colorectal cancer statistics, 2014. CA Cancer J Clin. 2014;64:104-17. doi:10.3322/caac.21220.
- Stoffel EM, Murphy CC. Epidemiology and mechanisms of the increasing incidence of colon and rectal cancers in young adults. Gastroenterology. 2020;158:341-53. doi:10.1053/j.gastro.2019.07.055.
- Jasperson KW, Tuohy TM, Neklason DW, Burt RW. Hereditary and familial colon cancer. Gastroenterology. 2010;138:2044-58. doi:10.1053/j.gastro.2010.01.054.
- DeSantis CE, Lin CC, Mariotto AB, et al. Cancer treatment and survivorship statistics, 2014. CA Cancer J Clin. 2014;64:252-71. doi:10.3322/caac.21235.
- Vogelstein B, Fearon ER, Hamilton SR, et al. Genetic alterations during colorectal-tumor development. N Engl J Med. 1988;319:525-32. doi:10.1056/NEJM198809013190901.
- Erstad DJ, Tumusiime G, Cusack JC Jr. Prognostic and predictive biomarkers in colorectal cancer: implications for the clinical surgeon. Ann Surg Oncol. 2015;22:3433-50. doi:10.1245/s10434-015-4706-x.
- Le Voyer TE, Sigurdson ER, Hanlon AL, et al. Colon cancer survival is associated with increasing number of lymph nodes analyzed: a secondary survey of intergroup trial INT-0089. J Clin Oncol. 2003;21:2912-9. doi:10.1200/JCO.2003.05.062.
- Kim YW, Kim NK, Min BS, Lee KY, Sohn SK, Cho CH. The influence of the number of retrieved lymph nodes on staging and survival in patients with stage II and III rectal cancer undergoing tumor-specific mesorectal excision. Ann Surg. 2009;249:965-72. doi:10.1097/SLA.0b013e3181a6cc25.
- Rahbari NN, Bork U, Motschall E, et al. Molecular detection of tumor cells in regional lymph nodes is associated with disease recurrence and poor survival in node-negative colorectal cancer: a systematic review and meta-analysis. J Clin Oncol. 2012;30:60-70. doi:10.1200/JCO.2011.36.9504.
- Bertelsen CA, Neuenschwander AU, Jansen JE, et al. Danish Colorectal Cancer G. Disease-free survival after complete mesocolic excision compared with conventional colon cancer surgery: a retrospective, population-based study. Lancet Oncol. 2015;16:161-8. doi:10.1016/s1470-2045(14)71168-4.
- Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S. Standardized surgery for colonic cancer: complete mesocolic excision and central ligation--technical notes and outcome. Colorectal Dis. 2009;11:354-64; discussion 64-5. doi:10.1111/j.1463-1318.2008.01735.x.
- Gangireddy VGR, Coleman T, Kanneganti P, et al. Polypectomy versus surgery in early colon cancer: size and location of colon cancer affect long-term survival. Int J Colorectal Dis. 2018;33:1349-57. doi:10.1007/s10350-007-9175-2.
- Hurwitz H, Fehrenbacher L, Novotny W, et al. Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med. 2004;350:2335-42. doi:10.1056/NEJMoa032691.
- Dienstmann R, Salazar R, Tabernero J. Personalizing colon cancer adjuvant therapy: selecting optimal treatments for individual patients. J Clin Oncol. 2015;33:1787-96. doi:10.1200/JCO.2014.60.0213.
- Dudley JC, Lin MT, Le DT, Eshleman JR. Microsatellite instability as a biomarker for PD-1 blockade. Clin Cancer Res. 2016;22:813-20. doi:10.1158/1078-0432.CCR-15-1678.

