Squamous Cell Carcinoma Excision from Right Forearm with Split-Thickness Skin Graft from the Thigh
Abstract
Skin is the largest organ by surface area of the body and is essential to prevent dehydration as the first barrier to infection, permit unrestricted movement, and provide a normal profile and appearance. A skin graft is a paper-thin piece of skin that has no fat or other body tissues attached and has been completely removed from its blood supply. Therefore, a skin graft can be transferred anywhere in the body as long as where placed, the so-called recipient site, does have a sufficient blood supply to nourish the skin until new blood vessels can grow into it within a short timeframe. Otherwise, if that does not occur, the graft will shrivel up and die. The downside even of a successful skin graft is the variable final color and inharmonious appearance of the skin, a tendency to contract possibly causing deformities especially limiting motion across joints, and similar healing issues at a second wound, that is the donor site of the graft itself. Nevertheless, this is a rapidly performed surgical procedure requiring but the simplest of instrumentation for the harvest of that graft that can then permit replacement of extensive skin deficiencies. In this video article, these virtues are displayed as a split-thickness skin graft is used to replace the skin missing following the removal of a large squamous cell skin cancer of the forearm.
Case Overview
This elderly woman presented with a long-standing, neglected, crusty, biopsy-proven squamous cell skin cancer of the top surface of her right forearm. Since larger than 2 cm in diameter, this would be a high-risk type of squamous cell skin cancer that has a high risk for metastasis or potential to spread to other parts of the body.1,2 As such, surgery would be the standard of care to try to remove all tumor cells by a wide excision into normal tissue about the tumor. The specimen obtained will always be reviewed later under the microscope to check all edges for any remaining tumor. If negative with no tumor seen, the chance of cure approaches 90% or more.2 If not removed at all, or if the edges still have tumor present, a squamous cell cancer will continue to grow where it began; but also can metastasize elsewhere, which could result in the death of the individual. Only for the extremely elderly or patients with other medical problems who would not tolerate the anesthesia for a major surgical operation would non-surgical treatment with radiation therapy be an alternate consideration.1,2
An operating room was used so that the patient would have a “twilight” sedation to make her pain free and comfortable.
To summarize the procedure in the video, an area extending about 10 mm into normal tissues all around the tumor of the right forearm was marked. This skin was cut around the tumor following those marks, and then down deep enough into the fatty tissues below to ensure that all tumor was removed. This left a large hole that could not be closed just by sewing together the surrounding skin, so another option had to be considered.
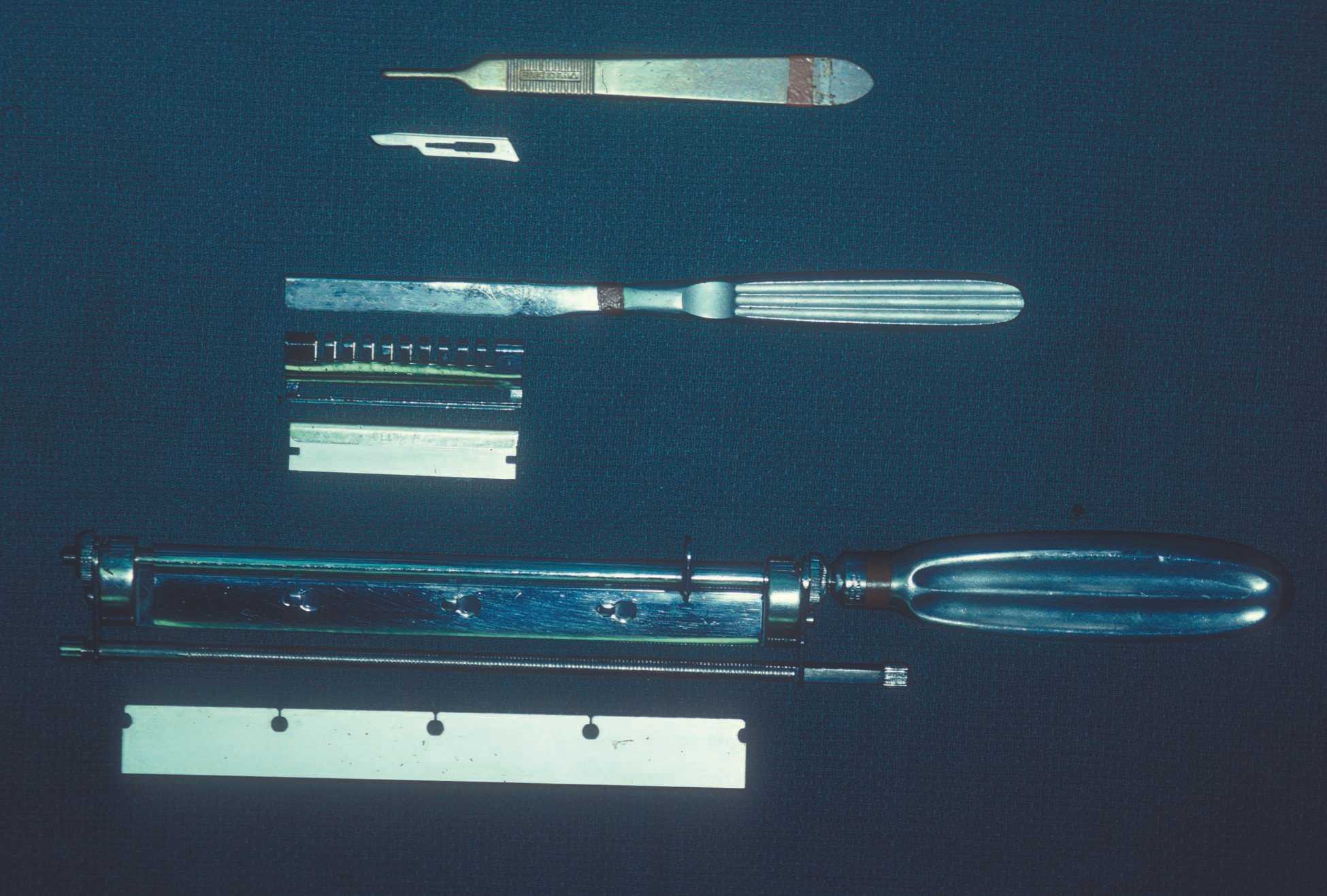
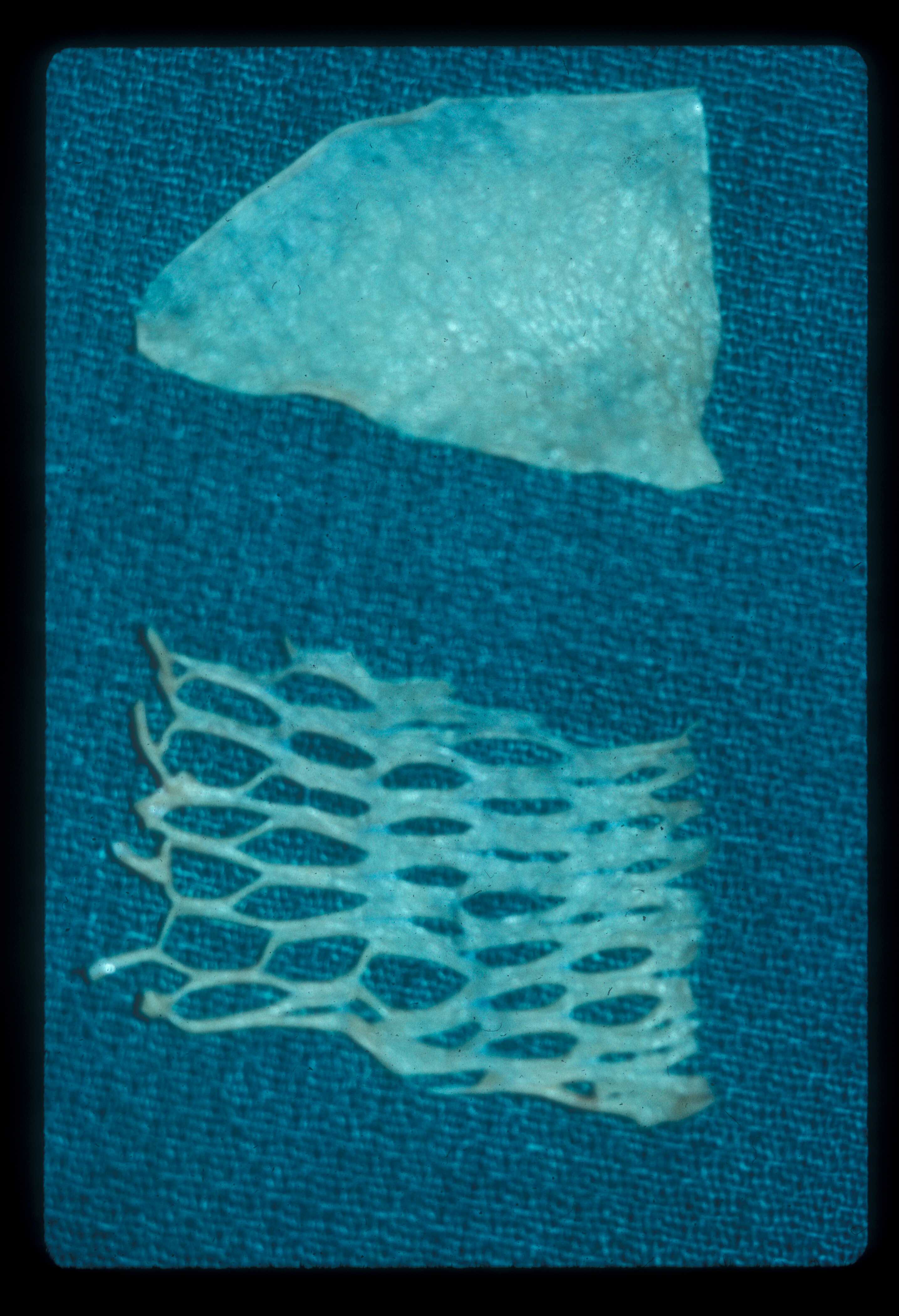
Because of her advanced age, her skin was very thin and fragile with minimal underlying fat tissue. Movement of that tissue with its blood supply intact, as what would be called a flap, was therefore considered impractical. Instead, to replace the missing skin, a skin graft was taken from her thigh as the best simple choice for her. Because no motorized dermatomes or skin harvesting machines were available to slice a thin layer of skin off her thigh much like a cheese slicer (i.e. Figure 1), instead a very sharp surgical knife was used to carve off the outer skin layer that would be the graft (i.e. Figure 2). Holes were pierced in the graft (i.e. Figure 3), which allows it to be spread apart to gain greater surface area dimensions; but also to permit drainage of any blood from the wound to come through them so that the graft is not lifted off the forearm before new blood vessels can grow into it to provide the necessary permanent blood supply. This step is called “pie-crusting,” analogous to that done by a baker to the top layer of the crust of a pie so that the steam created when baked can vent out through the holes and not explode the crust into pieces.
The harvested skin graft was stapled or sutured onto the forearm so that it would not move. A bulky dressing was next placed to stay on for a few days to prevent movement so that the graft would stick where fixed. The total time to obtain and place the skin graft was about a half hour with almost no blood loss, so the surgery was done as an out-patient allowing her to go home soon afterwards. The staples are customarily removed a week later as long as the graft seems to be “taking” by acquiring a pink color, which implies that circulation is being reestablished. Sometimes this can take several weeks to completely occur, until which time the graft could be grabbed and easily torn off the recipient site if one is not careful.
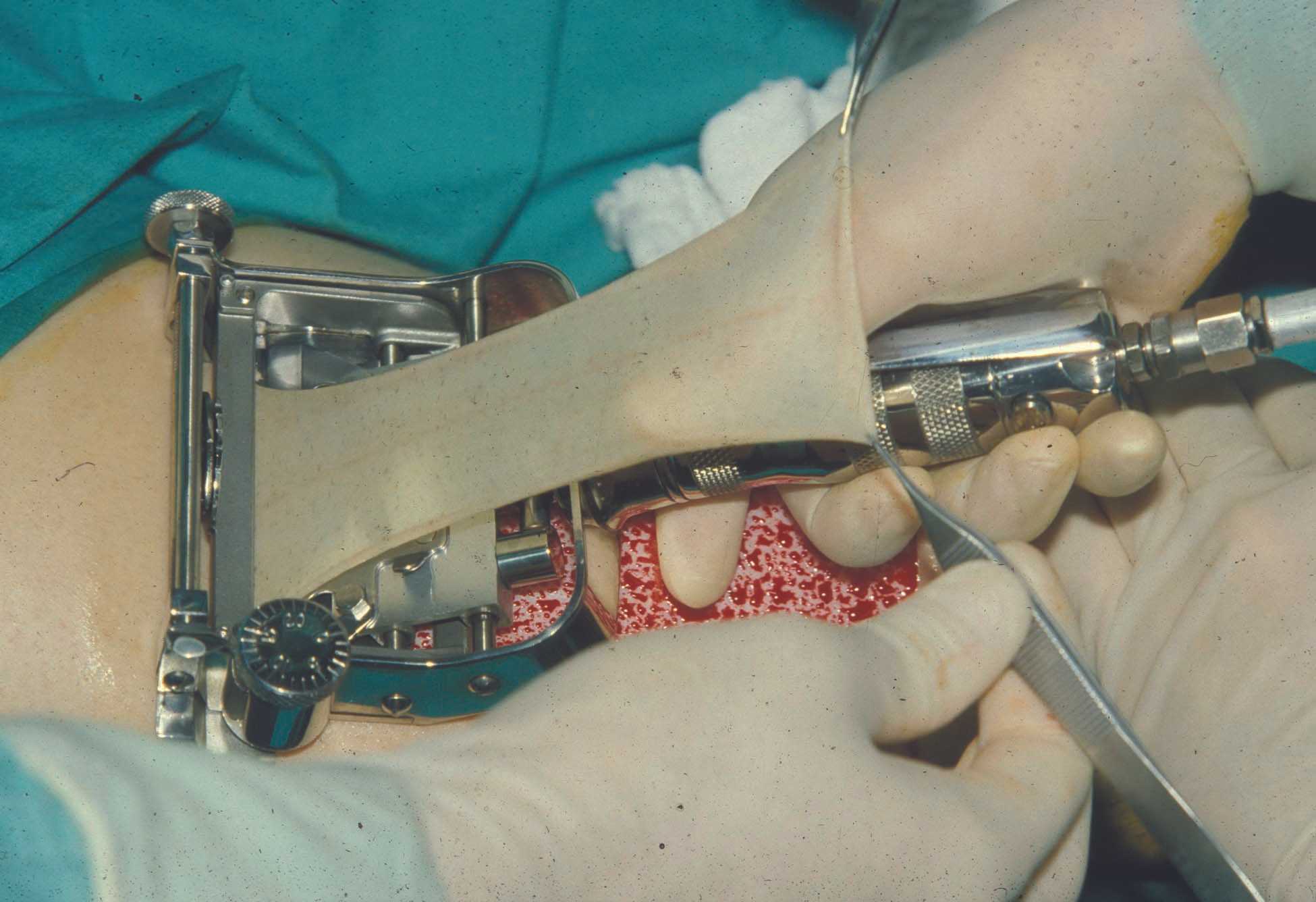
Figure 1. Motorized Brown dermatome allows rapid harvest of a split-thickness skin graft of predetermined thickness.
Discussion
Squamous cell skin cancer is the second most common type of skin cancer.2 Basal cell skin cancer is 4-5 times more common, and the number of these two found every year exceeds the number of all other cancer types combined.1,3
There are many risks factors for causing squamous cell skin cancer that are similar to basal cell skin cancer such as fair skin, use of tanning beds, age over 40, and genetics; but far most common is the extent of sun exposure leading often to what is called an “actinic keratosis,” which is considered a premalignant lesion.2,3
The most characteristic appearance of a squamous cell skin cancer is a slightly raised pink plaque that often is scaly and can have open sores or ulcerations (i.e. Figure 4). High-risk lesions include large or deep lesions as in the presented case, rapidly growing lesions, or recurrent lesions that have grown back for whatever reason.1,2 Unlike basal cell skin cancers where there is little risk of metastasis or spread away from the origin of the lesion,3 high-risk squamous cell skin cancers have a rate of metastasis of about 30% and even those that are low risk have a 2–6% incidence of metastasis.1,2 If that occurs, death is a possible outcome that should be incentive enough for the patient to want whatever additional surgery is needed to ensure total tumor removal as soon as possible.4 Since more tissue is usually taken than must-be-removed to obtain a cure, more often than not, a skin graft as done here, or a flap, will be necessary to allow healing of the skin.
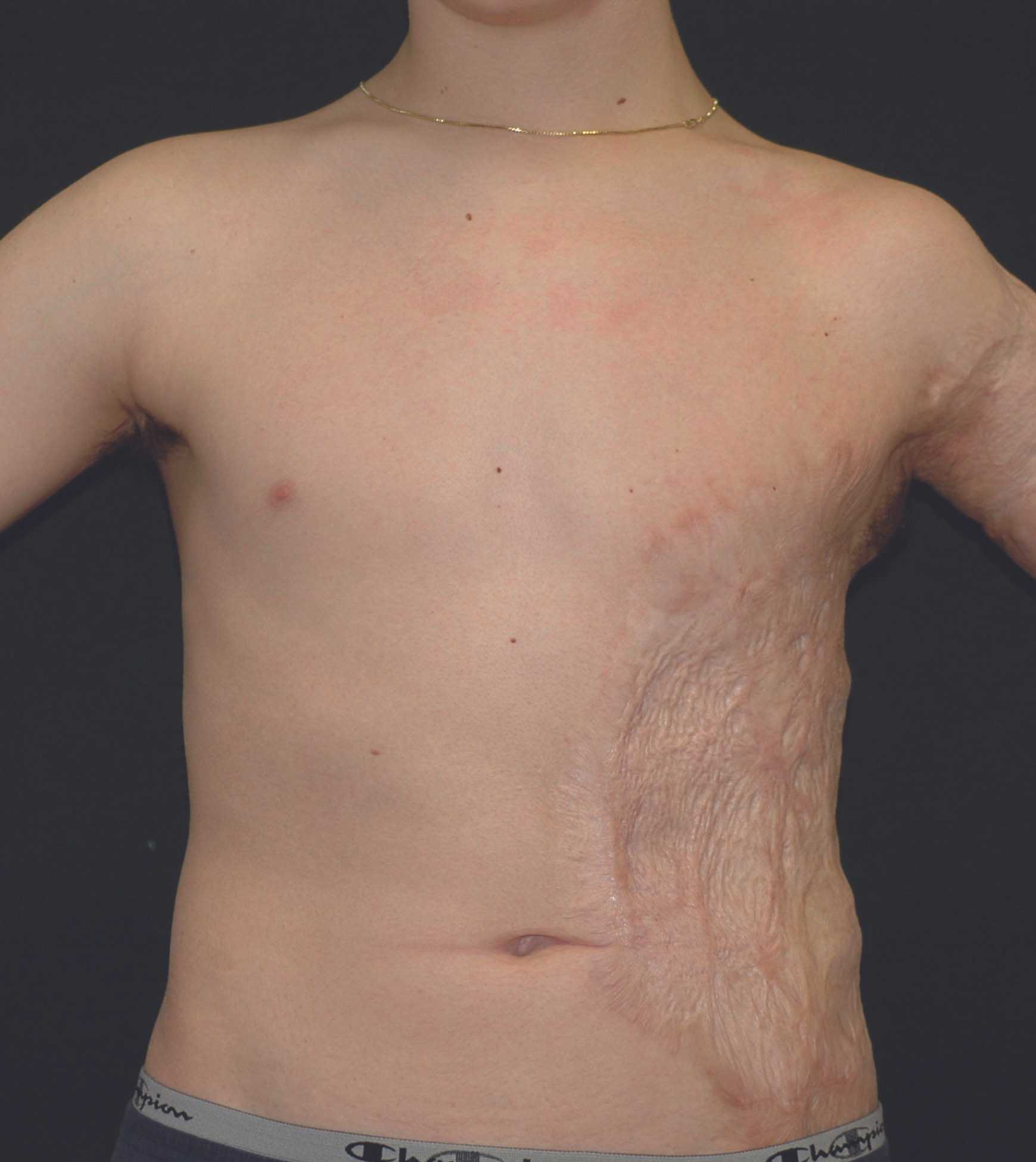
A simple way to get extra skin to cover any wound is to obtain and transfer a skin graft. Such use is well documented in Egyptian hieroglyphics, and even by the tile-maker’s caste in India centuries ago.5 When all the skin is removed from an area leaving the fat behind, this is called a full-thickness skin graft. This is most easily done with a surgical knife. If instead only the outer portion of the skin is separated, this would be called a split-thickness skin graft (i.e. Figure 2). The advantage of this option is that enough skin is left at the donor site that it will heal itself. Skin grafts may be taken from anywhere in the body, but an unappealing defect or scar will be left behind so it is best to use an inconspicuous location that is easily hidden especially by clothing (i.e. Figure 5). Since a skin graft has no blood supply, its survival relies on nutrients obtained from where it is placed, which must itself have a good blood supply. Thus, a skin graft sometimes cannot be used to cover for example exposed bone, and instead a flap that has tissues with their own blood supply would be preferable. Even when successful, a skin graft results in a suboptimal appearance (i.e. Figure 6), which might be devastating for a patient if used to cover any exposed regions such as the face.
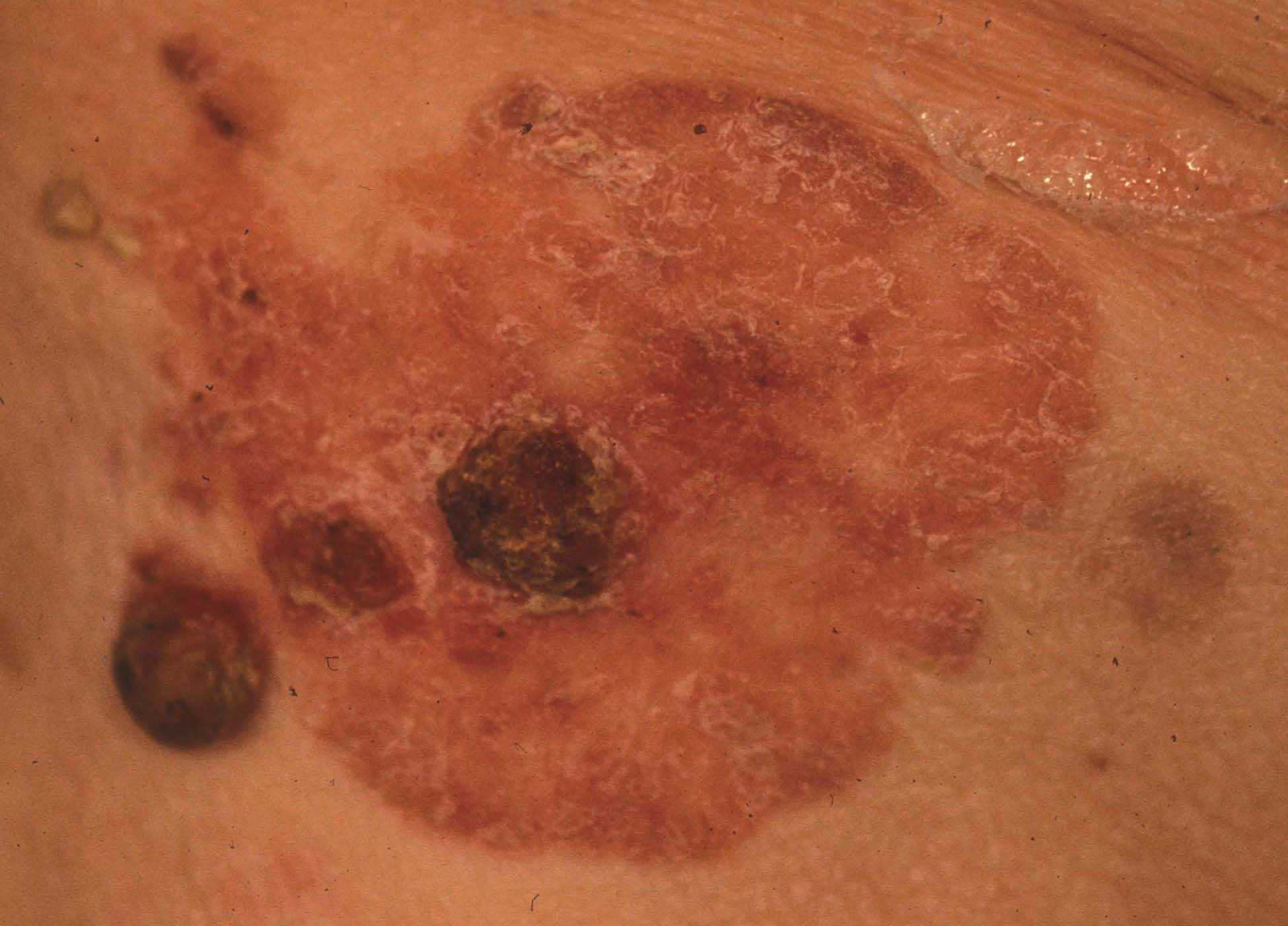
Figure 4. Common appearance of a squamous cell skin cancer as a pink plaque with a scaly or crusty surface.
Equipment
- Sharp surgical blades with special skin graft knife handles such as a Humby knife.
- Motorized dermatome for rapid, precise cutting of skin grafts.
- Scissors or skin mesher to create graft vent holes.
Disclosures
Nothing to disclose.
Statement of Consent
The patient referred to in this video article has given their informed consent to be filmed and is aware that information and images will be published online.
Acknowledgments
Kate Mertz, Surgical Technician, from Bowmanstown, Pennsylvania, was the first assistant for all surgery.
Citations
-
Mendez BM, Thornton JF. Current Basal and Squamous Cell Skin Cancer Management. Plast Reconstr Surg. 2018 Sep;142(3):373e-387e. doi:10.1097/PRS.0000000000004696.
-
Rudolph R, Zelac DE. Squamous cell carcinoma of the skin. Plast Reconstr Surg. 2004 Nov;114(6):82e-94e. doi:10.1097/01.prs.0000138243.45735.8a.
- Gulleth Y, Goldberg N, Silverman RP, Gastman BR. What is the best surgical margin for a basal cell carcinoma: a meta-analysis of the literature. Plast Reconstr Surg. 2010;126(4):1222-1231. doi:10.1097/PRS.0b013e3181ea450d.
- An Introduction to Mohs Micrographic Surgery. American Society of Dermatologic Surgery.
Available at: https://www.youtube.com/watch?v=W5Paup_-S4A&feature=youtu.be. 2017. -
Hallock GG, Morris SF. Skin grafts and local flaps. Plast Reconstr Surg. 2011 Jan;127(1):5e-22e. doi:10.1097/PRS.0b013e3181fad46c.