Airway Management: Techniques and Equipment
- Abstract
- Introduction
- General Overview
- Preparation and Equipment Check
- Standard Intubation and Difficult Airway Equipment Overview
- Direct Visualization with Intubation
- C-MAC Video Laryngoscope
- Bougie Intubation
- Laryngoscopes
- Fiber Optic Flexible Scope
- Cricothyroidotomy
- Closing Remarks
- Supplementary Materials
- Citations
Abstract
This video article discusses airway management techniques in trauma resuscitation. It outlines the preparation and equipment used in patients with impending airway failure that require airway protection and ventilatory support. We discuss the innovative airway towers used in the University of Chicago emergency room as well as the general approach to airway management. We also go over the different types of laryngoscopy, assist devices, and cricothyroidotomy surgical airway procedures.
Introduction
Clinicians generally classify airway management techniques into two categories: noninvasive (passive oxygenation, bag-valve-mask ventilation, and noninvasive positive-pressure ventilation) and invasive (supraglottic airways, endotracheal intubation, cricothyroidotomy, and tracheostomy).1 Trauma airways are particularly critical airways as these patients have the ability to deteriorate quickly from airway compromise and hemodynamic instability due to their traumatic injuries. We will describe a systematic approach to airway management in the trauma patient.
General Overview
In anticipation of an incoming trauma patient, preparation for airway management is a critical component of trauma resuscitation. All airway management situations should be performed as efficiently and safely as possible. Team and equipment preparation are key to facilitating this. In general, begin by assembling your team, identifying which individuals will be available and their roles (e.g, respiratory therapy, medical technicians, EMS/paramedics) in helping you control the airway.
Having a visible airway plan or guideline in the resuscitation/intubation area, along with a checklist, can greatly enhance coordinated efforts. These tools help ensure that all team members are on the same page, reduce the likelihood of errors, and streamline the process, especially in high-stress situations.
Be familiar with the ventilation system your department and what equipment your respiratory therapist (RT) will bring along. Setting up and managing ventilation after intubation, in the absence of an RT in your hospital, is the responsibility of the intubating doctor, anesthetist, or ED team until the patient has been discharged from the ED to the OR or intensive care unit. The intubating doctor or team should be familiar with the available airway and ventilation equipment and ensure that all the correct equipment is available prior to commencing intubation.
Familiarize yourself with where your airway and ventilation equipment is stored (traditional airway tackle box or airway trolley) and consider whether the storage layout could be optimized to improve safety and efficiency in your ED. We recommend storing all essential airway equipment on an airway trolley.2 This should have the material needed to secure the airway once established as well as key post-intubation equipment such as the end-tidal carbon dioxide monitor (EtCO2), suction, and a bag valve mask (BVM). A suggested approach is one used at the University of Chicago’s Trauma Center, which relies on an “Airway Tower” in order to ensure efficiency and quality control. Adjust your preparation as needed per your emergency medical services (EMS) reports if the information is provided prior to the patient’s arrival (e.g burn injury, extensive facial injuries, surgical airway intervention anticipation). Keep in mind that patients may appear stable on arrival yet quickly deteriorate during their clinical course during trauma resuscitations so it is suggested to always be prepared to manage a critical airway with all trauma resuscitations.
Preparation and Equipment Check
Ensure that your patient monitor is on and ready for the ancillary team to place necessary leads on the patient upon their arrival and obtain key vital signs including your oxygenation levels. It is essential to check your equipment for any faults or deficiencies prior to the patient’s arrival.
In anticipation of possible large-volume emesis or hemorrhagic airway, arrange the necessary components to suction the patient. Your suction canister and tubing should be checked to ensure they are working appropriately. Attach your Yankauer to your suction tubing and ensure all the valves and ports along the suction canister are closed and turn on the suctioning apparatus to ensure there are no leaks. Place the suction apparatus in a convenient location for you that’s easy to access when necessary. We suggest placing it within the suction packaging and tucked underneath the patient’s bed until it is needed.
Please keep in mind that some Yankauers require you to cover a small safety vent hole at the base in order to provide high-quality suctioning (some providers place tape over this covering in order to assist in covering the small hole, or you can use your thumb or index finger while suctioning).3
After assembling your suction equipment ensure all components of the BVM are available, including the detachable mask, bag valve, and oxygenation tubing. Elongate the bag as most are compressed for packaging and attach the tubing to your wall oxygen and start with 10–15 liters. Guidelines usually recommend 15 L per minute. Attach the mask to the valve and compress the bag as a test to ensure air is being provided as expected with each bag compression.
Bag-valve-mask ventilation is a crucial emergency skill. This fundamental airway management technique facilitates oxygenation and ventilation of patients until a more definitive airway can be established. It is particularly vital in situations where endotracheal intubation or other definitive airway control is not feasible.
Consider an oropharyngeal airway (OPA) or nasopharyngeal airway (NPA) also referred to as a nasal trumpet have available bedside if needed to augment oxygenation, but be cautious as significant (or suspected) facial or nasal injuries are a general contraindication to nasopharyngeal airway adjuncts because of potentially worsening existing injuries or causing damage to the cribriform plate.1 However it is a relative contraindication, when the doctor is unable to ventilate the hypoxic patient despite jaw thrust, OPA and experienced two-handed BVM an experienced team leader may choose to insert an NPA rather than allow hypoxic cardiac arrest. It is crucial to emphasize that while establishing a definitive airway is necessary, the team must avoid becoming task-focused on endotracheal tube (ETT) placement at the expense of maintaining adequate oxygenation and ventilation.
Standard Intubation and Difficult Airway Equipment Overview
Based on our experience at a high volume level 1 trauma center, our airway tower is constructed based on efficiency and most commonly needed intubation equipment. We will discuss the intubation process in subsequent sections, but first, we will go over what equipment to have and manners to arrange it. The most commonly used equipment and necessities observed during trauma airway resuscitations generally consist of quick and easy access to the following:
- An endotracheal tube (ETT)
- Laryngoscope (direct visualization laryngoscope or the video laryngoscope)
- Video laryngoscope
- 10-cc or 12-cc syringe
- Flexible stylet
- Nasal trumpet and/or oropharyngeal airways
- Bag valve mask
The first drawer consists of direct visualization laryngoscope blades as well as the attachable handles, OPAs, NPAs, 10- or 12-cc syringes, various-sized ETTs, a flexible stylet, and a 60-cc syringe (to allow inflation and deflation of supraglottic airways placed in the field via EMS prior to their removal). This first drawer is designed to provide assistance in a stepwise progression of airway management from top to bottom and left to right, with adjuncts becoming more advanced alongside increasingly necessary advanced airway management (e.g., the adjuncts for bag valve mask assistance such as the OPA are available on the left, followed by the equipment needed to intubate in a stepwise fashion as you go towards the right of the drawer). For example, if you have an assistant, you can ask them to start from the right and organize your ETT and stylet while you set up your laryngoscope equipment.
The second drawer consists of equipment needed postintubation such as an ET tube holder (strap method) and CO2 detector (color change), capnography.1
The third drawer consists of various-sized ET tubes and extra direct visualization laryngoscope blades.
The fourth drawer consists of the supraglottic airways. Current, correct terminology is: supraglottic airway devices (SADs), which include the first generation laryngeal mask airway (LMA) and the second generation King airway. While SADs are most commonly used in the operating room (OR) for elective surgery they have a range of important uses out with the OR including airway management in cardiac arrest and prehospital by practitioners not skilled with endotracheal intubation. In addition they are essential in management of difficult airways where they can facilitate ventilation when BVM with OPA/NPA has been unsuccessful and in the failed intubation scenario oxygenation/ventilation can be maintained via SAD whilst the team prepares an alternative intubation strategy such as front of neck access or fiber optic intubation using the SAD. It is generally agreed that second generation SADs perform better for resuscitation, pre-hospital care and difficult airway management.10-11
Ultimately an ETT will providea definitive airway, protecting again aspiration and enabling optimal ventilation.5
The fifth drawer contains extra supplies such as suction canisters, suction tubing, Yankauers, nasal cannulas, and masks.
The sixth and final drawer consists of equipment needed for difficult airways. This kit would also be used in the unanticipated difficult airway. Anticipate the use of difficult airway equipment for those you suspect have had crush injuries to the neck, expanding hematomas, extensive facial injuries, or known foreign bodies obstructing the airway. This drawer contains items such as surgical scrub cap, headlamp, sterile gloves, number 10-blade scalpel, a cricothyroidotomy tray, tracheostomy tube, nasal ETT, and atomizer.
Direct Visualization with Intubation
Preoxygenation is a process that displaces nitrogen with oxygen in air spaces to extend the safe apnea time.1 It should be initiated in all patients as soon as it is determined a patient will require intubation. Using a BVM or non-rebreather (NRB), administer 100% oxygen delivered at 15 L/min. A nasal cannula can also be used with BVM or NRB to maximize oxygenation.1 Use of oxygen via nasal cannula during preoxygenation and intubation attempts can prolong the apnoea time and is recommended by the DAS. Additional adjuncts including OPA, NPA, jaw thrust, and the chin lift maneuver may be used to optimize preoxygenation.
Nasal high-flow oxygen (NHFO) is one of the effective preoxygenation techniques that delivers heated and humidified oxygen at high flow rates, improving oxygenation and patient comfort. It extends the safe apnea time during intubation by maintaining high alveolar oxygen levels and positive airway pressure. This makes NHFO particularly valuable for patients with respiratory challenges.
Position the patient in the “sniffing” position with the lower neck flexed and the head extended for the optimal angle. A neck roll may be placed under the patient’s neck to help. A 20–25 degree head-up position improves the view, extends the apnea time, and is essential in obese or pregnant patients. Excessive neck extension and the head tilt-chin lift maneuver are contraindicated if there is a history suggesting spinal injury. In these cases, the following techniques can be used to facilitate ventilation: jaw thrust maneuver, manual in-line stabilization, use of video laryngoscopy, and rapid sequence intubation.
Remove any dentures or foreign bodies from the oropharynx that may obscure your view and suction any visible secretions with your Yankauer.
With the laryngoscope (Mac or Miller blade) held in the left hand, use the right thumb and index finger to scissor open the patient’s mouth. Insert the laryngoscope into the mouth, scooping the tongue underneath the blade in a right-to-left direction, and advance into the larynx. Once the arytenoids are in view, lift the epiglottis. Using the right hand, insert the ETT with stylet, following the curve of the blade, and visualize the end of the ETT passing through the vocal cords until the cuff is below the cords. An assistant should be available and ready to remove the stylet. Initially, the stylet should be withdrawn very slightly, allowing the ETT to pass through the cords to the correct placement (black line at the cords). While the doctor holds the ETT and monitors the larynx, the assistant should carefully withdraw the stylet. It is well documented that the action of withdrawing a stylet can displace the ETT from the larynx. Remove the laryngoscope while holding the ETT in place and inflate the balloon. Ideally, the cuff pressure should be between 20 and 30 cm H2O. The amount of air needed to achieve a pressure of 20 cm H2O is small, ranging from 2.6 mL for a 7.0-mm ETT to 3.3 mL for an 8.5-mm tube. Secure the ETT and connect it to an oxygen source (e.g., BVM or ventilator).
Check for ETT placement by auscultation, observing tube condensation, visualizing equal and bilateral chest rise, noting color change on a colorimeter from purple to yellow, or using an EtCO2 detector. An EtCO2 detector should be connected to the circuit during preoxygenation or upon arrival if the patient comes with a supraglottic airway device (SAD) inserted by the prehospital team.
C-MAC Video Laryngoscope
Video laryngoscopy allows transmission of the view via an external monitor for enhanced and shared visualization. It provides an advantage in patients with difficult airway anatomy. Videolaryngoscopy has become the recommended first-line approach for trauma airways when available to provide increased chances of first-pass intubation. Become familiar with the video laryngoscope equipment available in your department, whether it is the C-MAC, Glidescope, or another brand.9 The C-MAC is one of the most commonly used devices.
The GlideScope video laryngoscope and the C-MAC have key design differences, and thus slightly different techniques may be needed to achieve glottic exposure. The C-MAC has a blade shape much like a standard Macintosh curve, allowing for a conventional approach similar to direct laryngoscopy. In contrast, the GlideScope video laryngoscope blade has a 60-degree curvature. Although the hyperangulated curvature affords improved glottic exposure in difficult airways, it also requires the use of a specially designed curved rigid stylet (GlideRite stylet) to facilitate the direction of the tracheal tube to the laryngeal inlet.4
In order to facilitate efficiency during the process consider placing a few key pieces of airway equipment (Bougie, MAC3 or 4, 7.0 or 7.5 ETT, 10-cc syringe, flexible stylet, hyperangulated D-blade) on the tower holding the video laryngoscope in order to provide ease of access. Consider that not all brands of video laryngoscope are mounted on a stand, some are wireless, no stack and would be stored in the airway trolley.
First, check to make sure all equipment and wires are connected and working properly to ensure smooth intubation. The technique used in video laryngoscopy is similar to that of direct laryngoscopy. Place the camera modulator into the laryngoscope blade you have chosen and test it to ensure the output is clear and focused. However, once the blade is inserted into the oropharynx, direct your attention towards the external monitor. Visualize the ETT going through the vocal cords just as in direct visualization and confirm the placement.
Video-assisted laryngoscopy also has the added advantage of allowing the use of a hyperangulated blade. The sharper, more acute angle of the blade allows the user to visualize more anterior or displaced airways. Masses, trauma, hematomas, or anatomic variations are some of the causes of displaced airways. When using a hyperangulated D-blade, you must use a rigid stylet that follows the angle of the blade.1
Despite manufacturers’ claims of antifog capabilities, fogging of video laryngoscope blades is common. Prewarming the blade by immersing it in warm water or using a warming device can help. Applying compatible antifog solutions or wipes is also effective. Ensuring the blade is thoroughly dried after cleaning prevents moisture buildup. Regularly checking and reapplying antifog measures as needed can maintain a clear view.
Bougie Intubation
The gum elastic Bougie is an important adjunct for difficult intubations in which the glottis cannot be adequately visualized. It is found on the side of all of our airway carts readily available. Its design allows it to be used with any of our laryngoscopes. The plastic introducer is long and flexible with an angulated tip. The angulated tip allows the bougie to maneuver to locate anteriorly located cords. Once inside the trachea, the operator should be able to find the tip of the angulated bougie moving against the tracheal rings confirming the correct location.6 The ETT can then be loaded onto the proximal end of the bougie and into the cords blindly. The ETT can also be preloaded onto the bougie. The bougie can be bent to follow the curvature of any of our laryngoscopes and used as a backup adjunct.
Laryngoscopes
Three common laryngoscope blades that we use are the Macintosh, Miller, and the hyperangulated D-blade. Each blade contains a light source connected to a handle. The Mac and hyperangulated blades can be used with video laryngoscopy, while the Miller blade is to be used exclusively for direct laryngoscopy.
The Mac blade is a curved blade designed to be inserted into the vallecula and indirectly lift the epiglottis upward. The Miller blade is a straight blade designed to be inserted posterior to the epiglottis in the larynx and directing the epiglottis upward. The hyperangulated blade has a 60-degree curvature designed to give better visibility with more anterior airways.7
Fiber Optic Flexible Scope
The fiber optic A scope allows for direct visualization and intubation in an awake trauma patient with anatomy or pathology that would make standard intubation challenging. Several patient populations in which awake intubation may be the best approach include burn victims with inhalation injury, penetrating neck injuries, expanding hematomas, and limited neck mobility. If you anticipate a difficult endotracheal intubation or rescue oxygenation with BVM, fiberoptic awake intubation should be considered. The fiberoptic scope allows for the visualization of the airway to assess for swelling, bleeding, or pathology and also for nasal intubation to avoid unstable oropharyngeal pathology.1
For an awake fiber optic intubation (AFOI) to be performed safely, with the patient remaining awake and spontaneously ventilating, adequate topicalization is required. Adequate topicalization is important to avoid gagging and coughing, which is essential and time-consuming, especially in agitated, confused, hypoxic trauma, or critically unwell patients. Glycopyrrolate 4 µg/kg given intramuscularly an hour before intubation dries mucus membranes, which both increases the efficacy of topical anesthesia and improves intubating conditions by decreasing secretions. Alternatively, intravenous glycopyrrolate may be injected in the emergency department, although unwanted side effects such as tachycardia may be more problematic.
Sometimes, an atomizer alone cannot adequately anesthetize the larynx (coughing may occur when the scope/endotracheal tube touches the larynx during intubation). Nebulized lidocaine can achieve this but is time-consuming. The “spray as you go” technique is commonly used and involves injecting lidocaine onto the larynx down the working channel of the scope. Using a syringe and epidural catheter down the channel of the scope makes this more accurate. Another option is the transtracheal route, but this might not be feasible with neck trauma or hematoma. Nerve blocks are also available but are tricky unless performed by skilled personnel and are unlikely to be possible with distorted neck anatomy in trauma. Another low-skill method, which is not well described, is to insert a nasopharyngeal airway (NPA) and inject lidocaine down it until the patient no longer coughs, suggesting an adequately anesthetized larynx.12-13
Once properly prepped, insert the tip of the scope into the nasal canal, guiding it along the floor of the canal. Follow the pharynx down until the vocal cords come into view. If airway swelling or smoke inhalation is anticipated, the ETT may be preloaded on the scope. Advance the tube through the vocal cords, visualizing on the Ambu screen. Fiber optic intubation will usually require a smaller ETT.
Constant talking and calming of the patient will be required by another person familiar with such procedures. A SAD with a fiberscope can be an excellent rescue tool in some cases. Potential uses include intubating via the SAD in the unconscious trauma patient who arrives from prehospital care with a working SAD in situ. Removing a reliable airway poses a risk of losing it as swelling may have developed subsequent to SAD insertion. Consider exchanging for an ETT using an exchange catheter and fiberscope. The SAD could be left in situ for oxygenation/ventilation while front-of-neck access (FONA) is secured if facial trauma/swelling is severe. More commonly, intubation via SAD is an essential part of the failed intubation algorithm. After three failed attempts but with the ability to ventilate, the SAD should be inserted, and then intubating using the scope via the SAD is an option when waking the patient is not feasible.
It is important to mention that using a fiberscope is a tricky skill, and practitioners should practice on a trainer before practicing under close supervision on an anesthetized patient in the OR. Additionally, in an airway soiled with blood, AFOI is unlikely to be possible as the view will be constantly obscured by blood.
Cricothyroidotomy
When all adjuncts have failed to establish a secure airway, a surgical airway must be established. You should be prepared for a cricothyroidotomy as a last resort backup for any intubation. The most important step of any procedure is preparation. Equipment needed for cricothyroidotomy includes a 6.0 ETT or size 6 Shiley tracheostomy tube, Bougie, 12-cc syringe, and a cricothyroidotomy tray kit (includes 11 blade scalpel, dilator, skin hooks, curved hemostat, scissors, and forceps).
Locate the cricothyroid membrane between the thyroid and cricoid cartilage and stabilize the two cartilages with the non-dominant hand. Using a number 10 or 11 scalpel, make a 1–2-inch vertical incision in the midline through the skin and subcutaneous tissues. Now make a horizontal incision through the cricothyroid membrane. Place the back end of the scalpel handle through the incision to widen it. You can also use a skin hook and hemostat to open the incision. Place a bougie through the opening aiming inferiorly. Place a size 6 ETT or tracheostomy tube over the Bougie through the opening sliding it inferiorly. Remove the Bougie. Secure the tube and confirm the placement. The alternative option is to use the Shiley tube with the attached stylet instead of the bougie.8
Closing Remarks
Airway management is the first step in trauma resuscitation. In general, airway management always begins with preparation and anticipating the worst-case scenario. At the University of Chicago, our airway carts allow us to always have all of our supplies readily available for emergent and trauma situations. After you have located all of your equipment and decided which medications to use, we move on to preoxygenation with the techniques discussed. There are several intubation techniques that can be used for any scenario you find yourself in. Be sure to familiarize yourself with direct laryngoscopy, video laryngoscopy, AFOI, and when all else fails, cricothyroidotomy surgical airways. Lastly, always confirm the placement of your airway device.
Supplementary Materials
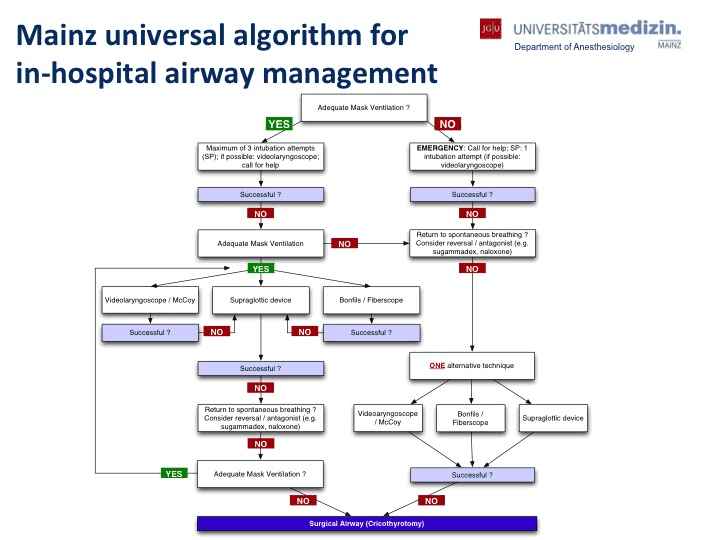
Figure 1. Mainz Universal Algorithm for In-Hospital Airway Management. Ott T, Truschinski K, Kriege M, et al. [Algorithm for securing an unexpected difficult airway : User analysis on a simulator]. Anaesthesist. 2018 Jan;67(1):18-26. German. doi:10.1007/s00101-017-0385-2.
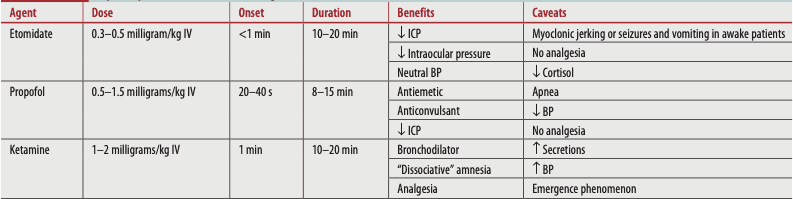
Table 1. Rapid-Sequence Intubation Induction Agents. Tintinalli JE, et al. (2020) Tintinalli's emergency medicine: a comprehensive study guide (9th edition). New York: McGraw-Hill Education.
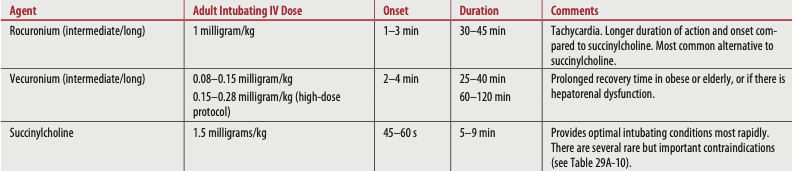
Table 2. Rapid-Sequence Intubation Paralytic (Neuromuscular Blocking) Agents. Tintinalli JE, et al. (2020) Tintinalli's emergency medicine: a comprehensive study guide (9th edition). New York: McGraw-Hill Education.
For further information on rapid-sequence intubation agents, please see the Pharmacology for Rapid Sequence Intubation (RSI) Airway Management in Trauma Patients article by Laura Celmins, PharmD, BCPS, BCCCP.
Citations
- Tintinalli JE, et al. (2020) Tintinalli's emergency medicine: a comprehensive study guide (9th edition). New York: McGraw-Hill Education.
- Flint LM (2008) Trauma: contemporary principles and therapy. Wolters Kluwer Health/Lippincott Williams & Wilkins.
-
Cox R, Andreae M, Shy B, DuCanto J, Strayer R. Yankauer suction catheters with "safety" vent holes may impair safety in emergent airway management. Am J Emerg Med. 2017 Nov;35(11):1762-1763. doi:10.1016/j.ajem.2017.04.009.
-
Mosier J, Chiu S, Patanwala AE, Sakles JC. A comparison of the GlideScope video laryngoscope to the C-MAC video laryngoscope for intubation in the emergency department. Ann Emerg Med. 2013 Apr;61(4):414-420.e1. doi:10.1016/j.annemergmed.2012.11.001.
-
Frerk C, Mitchell VS, McNarry AF, et al. Difficult Airway Society intubation guidelines working group. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth. 2015 Dec;115(6):827-48. doi:10.1093/bja/aev371.
- Kaul V. All that bladerdash. Crit Care Now. 2020.
- Cameron P, et al. (2011) Textbook of adult emergency medicine e-book (3rd edition). Churchill Livingstone.
-
Hansel J, Rogers AM, Lewis SR, Cook TM, Smith AF. Videolaryngoscopy versus direct laryngoscopy for adults undergoing tracheal intubation: a Cochrane systematic review and meta-analysis update. Br J Anaesth. 2022 Oct;129(4):612-623. doi:10.1016/j.bja.2022.05.027.
-
Apfelbaum JL, Hagberg CA, Connis RT, et al. 2022 American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway. Anesthesiology. 2022 Jan 1;136(1):31-81. doi:10.1097/ALN.0000000000004002.
-
Cook TM, Kelly FE. Time to abandon the 'vintage' laryngeal mask airway and adopt second-generation supraglottic airway devices as first choice. Br J Anaesth. 2015 Oct;115(4):497-9. doi:10.1093/bja/aev156.
-
Sole ML, Su X, Talbert S, et al. Evaluation of an intervention to maintain endotracheal tube cuff pressure within therapeutic range. Am J Crit Care. 2011 Mar;20(2):109-17; quiz 118. doi:10.4037/ajcc2011661.
-
Bhalotra AR. A Simple Method of Topicalisation to Facilitate Awake Fibreoptic Nasotracheal Intubation: Experience at a Tertiary Care Hospital. Turk J Anaesthesiol Reanim. 2018 Aug;46(4):333-334. doi:10.5152/TJAR.2018.68984.
-
Ahmad I, El-Boghdadly K, Bhagrath R, et al. Difficult Airway Society guidelines for awake tracheal intubation (ATI) in adults. Anaesthesia. 2020 Apr;75(4):509-528. doi:10.1111/anae.14904.