Corneal Staining with Fluorescein
Abstract
Patient ocular complaints often center around discomfort, foreign body sensation, and/or recent trauma. Determining the cause of the ailment is not always straightforward, and the use of fluorescein can provide valuable information that aids in clinical diagnosis. Many corneal conditions and emergencies can be identified with the aid of fluorescein such as corneal erosion, superficial punctate keratitis, corneal abrasion, foreign bodies, and tracking patterns of foreign bodies. This article and video will demonstrate proper technique to instill fluorescein and examine ocular tissues, as well as some examples of staining defects characteristic of compromised ocular tissues.
Indications
Indications include:1,2,3
- Dry eye
- Recent trauma
- Unspecific discomfort
- Contact lens discomfort
- Goldmann tonometry
Diagnoses Where Staining with Fluorescein is Useful
The following is a list of diagnoses where staining with fluorescein is useful:1,2,3
- Conjunctivitis: fluorescein may help with more definitive diagnosis between viral, bacterial, or allergic conjunctivitis
- Cornea or conjunctival abrasion
- Superficial punctate keratitis (SPK)
- Epithelial basement membrane dystrophy (EBMD)
- Various contact lens fitting problems
- Tear break up time
- Foreign body
- Ulceration
- Ruptured globe (Siedel’s test)
- Herpetic keratitis
Additional Examples of Various Ocular Conditions
Some examples of various ocular conditions can be seen in Figures 1-4. These photographs from the slit lamp were taken by the author.
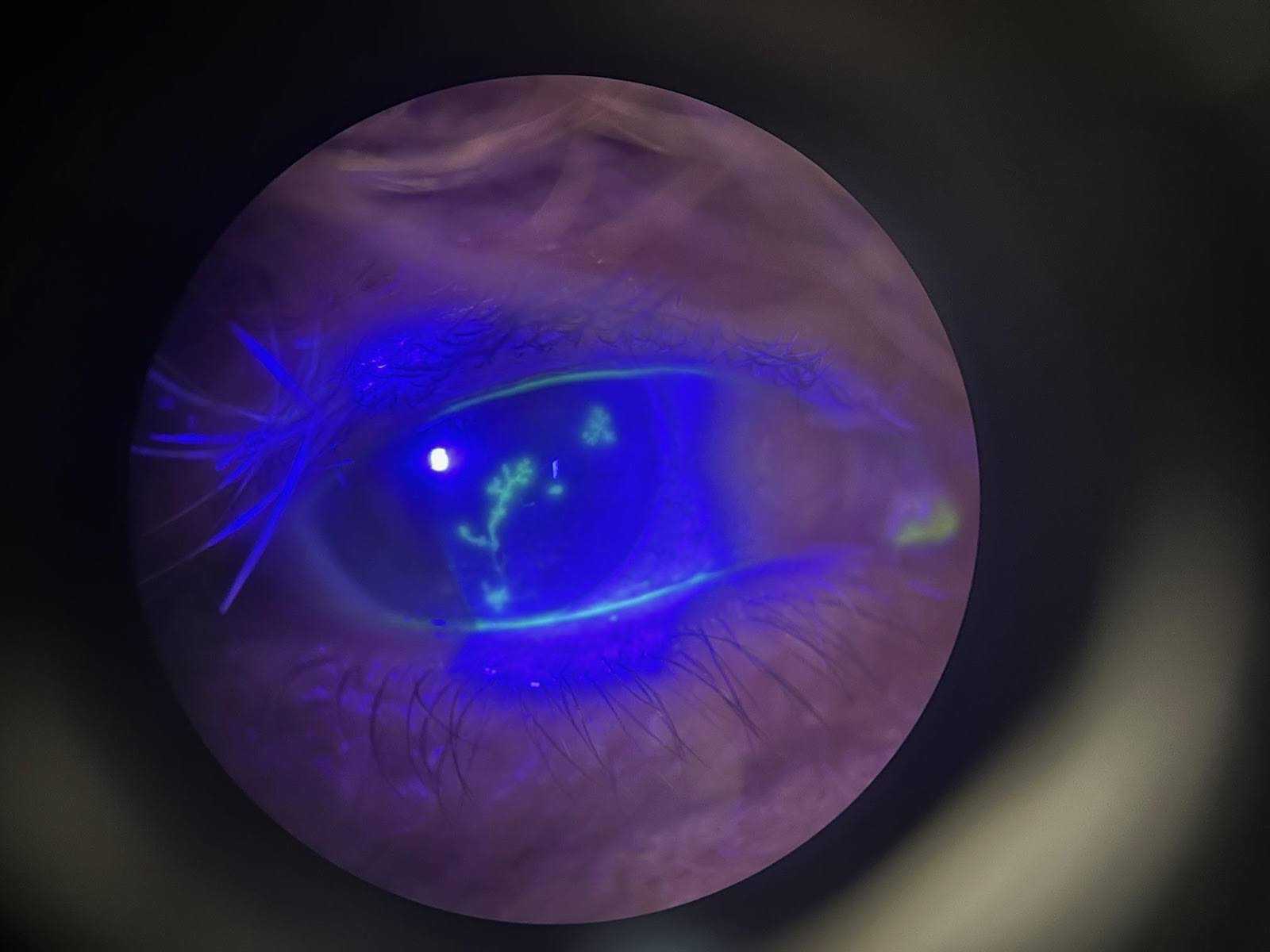
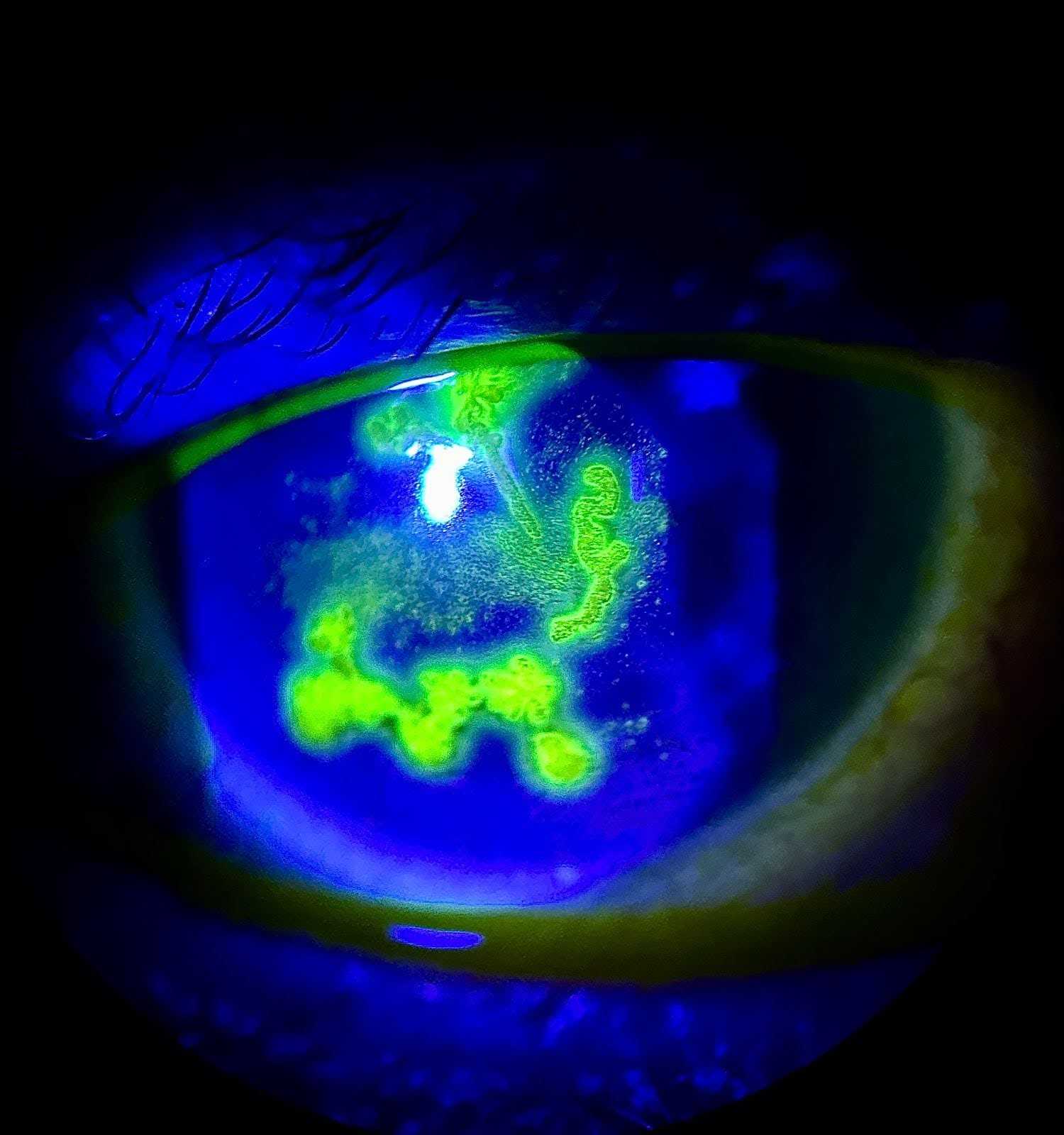
Figure 1. HSV in different patients showing the difference in acute presentations.

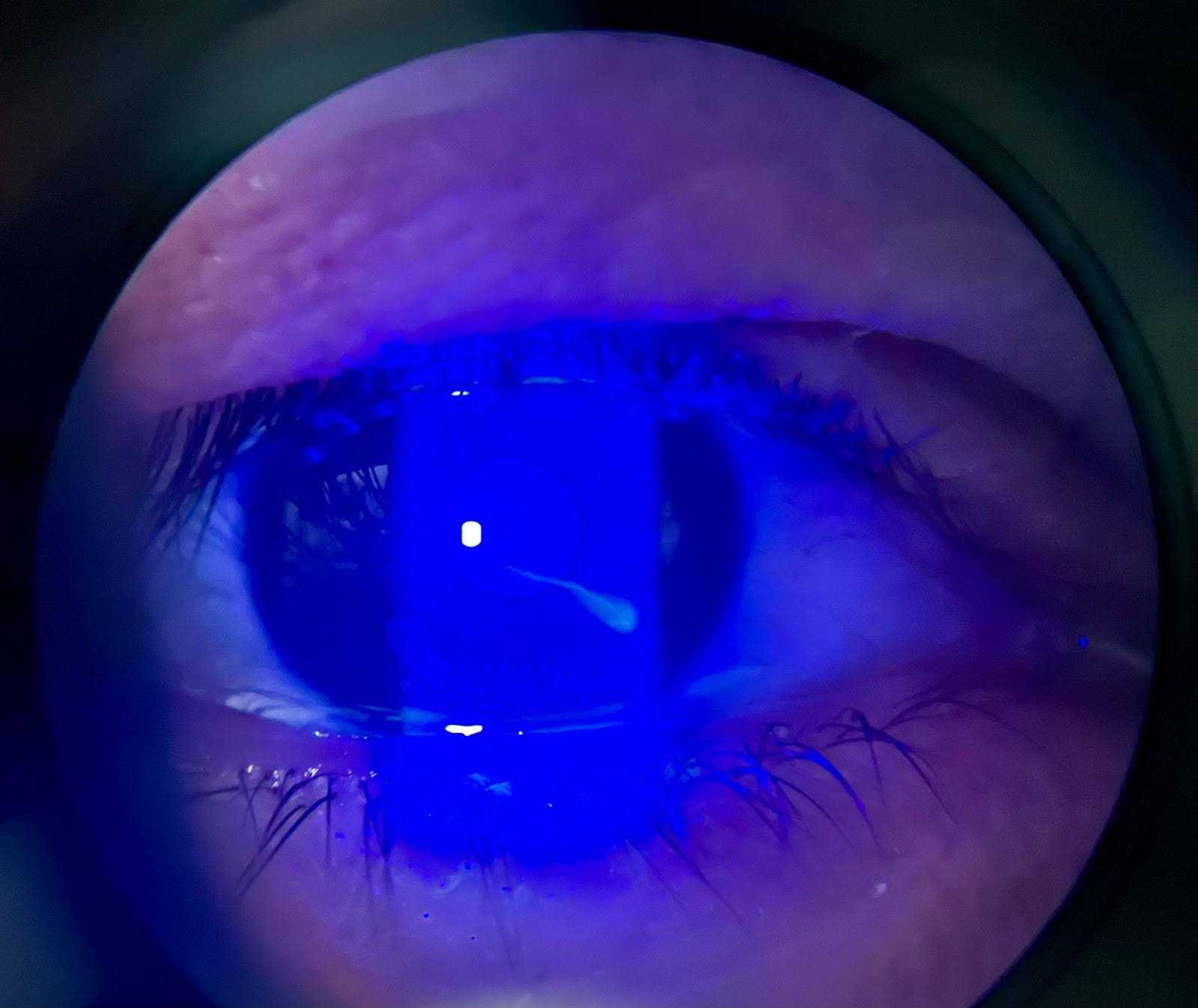
Figure 2.Corneal abrasions due to blunt trauma (Left) vs linear scratches (Right).
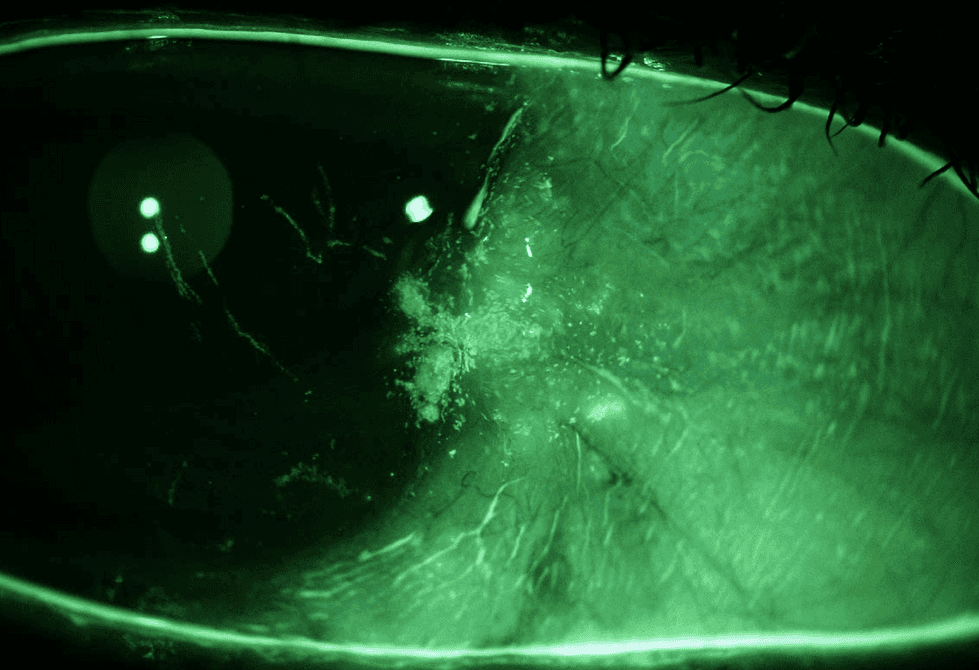
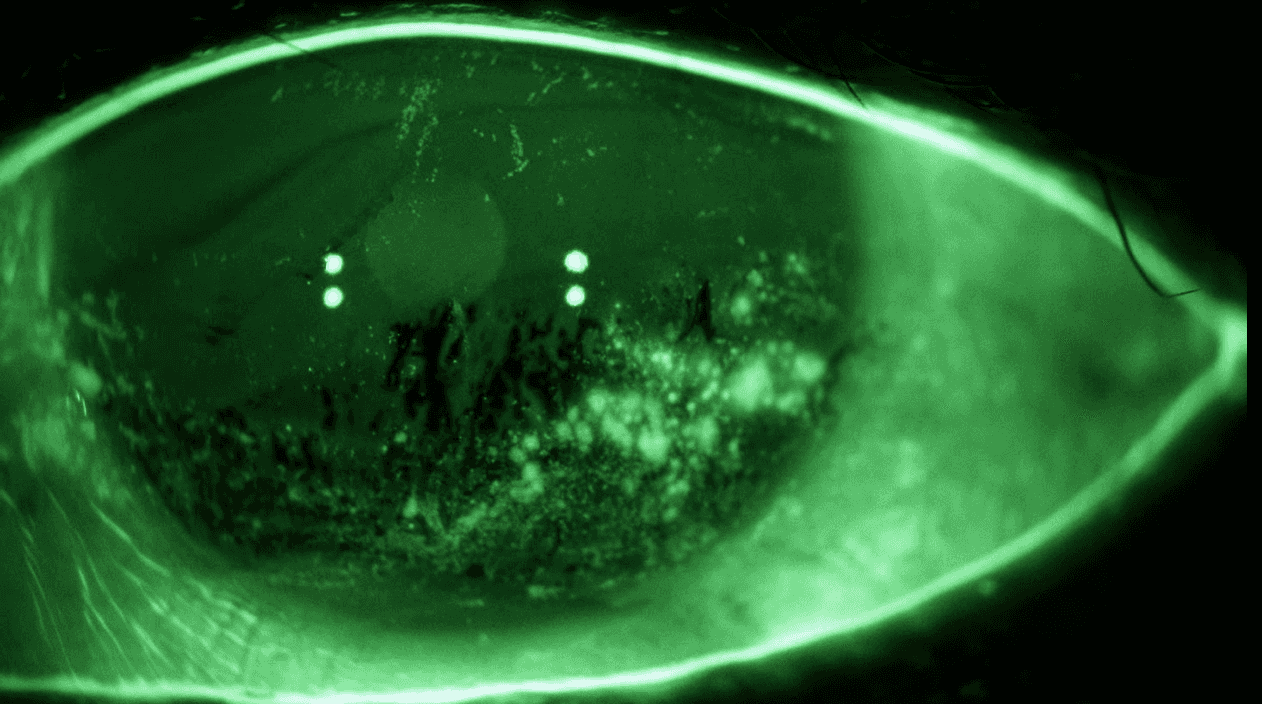
Figure 3. Right and left eyes of the same patient. Left) Right eye SPK in the area between the cornea and pterygium. Also note linear abrasions on the cornea. Right) Left eye severe SPK, positive and negative staining due to poor tear film also visible.
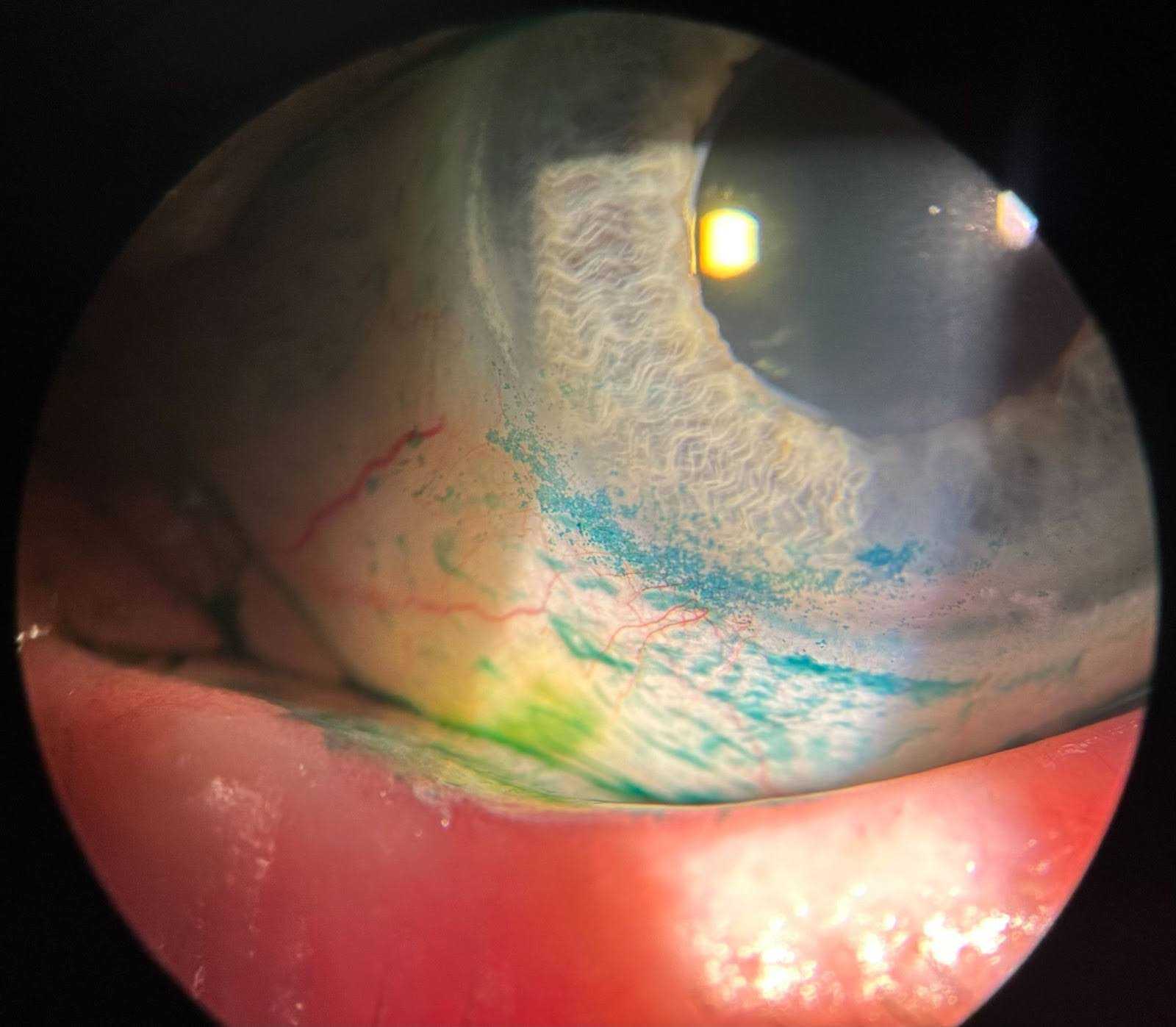
Figure 4. Example of conjunctival staining with lissamine Green. Patient has exposure keratitis (blue staining on conjunctiva and cornea) due to ectropion (eyelid folding away from the globe). Note white light used not a cobalt filter.
Equipment
The following equipment is used:1,2,3
- Sodium fluorescein test strip. Liquid fluorescein in certain clinics (mostly used for Goldmann Tonometry as it is combined with topical anesthetic).
- Drop to help elute the fluorescein test strip. Saline is recommended; however, in clinical practice, proparacaine is sometimes used.
- Blue light (cobalt blue filter) and magnification system (standard slit lamp configuration at least 10x magnification).
Exam Flow
The usual pattern for the exam flow is as follows:1,2,3
- Careful case history will determine likely diagnosis.
- Educate the patient and obtain consent about the procedure and what to expect. Confirm the patient is not pregnant and has no allergies to dyes or anesthetic (commonly available: proparacaine or tetracaine). In traumatic situations, patients will be in severe pain and are unlikely to be able to open the eye without topical anesthetics first.
- Elute fluorescein strip over a trash can. Allow excess to drip off into the trash can.
- Place impregnated fluorescein strip on the inferior aspect of bulbar conjunctiva. Do not paint the conjunctiva; use as little of fluorescein as possible. Using too much fluorescein will prevent accurate diagnosis. Correct technique dictates waiting one minute after instillation before examining ocular tissues to allow for excess fluorescein to drain.2 To avoid corneal abrasions, never apply impregnated strip to the cornea.2
- Dim room illumination and evaluate ocular tissues using blue light and magnification.
Potential Complications
Complications include:1,2
- Abrasion if fluorescein strip scratches the cornea.
- Allergy to fluorescein.
Discussion
Command of staining ocular tissues with vital dyes is an essential ophthalmologic technique due to its diagnostic capability in both acute traumatic conditions and chronic disease. Fluorescein is not the only vital dye but it is the most commonly used as its mechanism of action is to penetrate intercellular space.1 Fluorescein absorption maximum is around 490 nm and emission maximum is around 520 nm.1 This is why we shine blue light to see a green lesion. Other examples of dyes include lissamine green and rose bengal, but their limited availability and more specialized use makes them less common. Rose bengal evaluates preocular tear film, and lissamine green stains devitalized cells.1 A perfect example of using multiple dyes is in the case of Herpes keratitis, if one were to stain with both fluorescein and rose bengal, the center of the lesion “end bulbs” stain with fluorescein, while the peripheral aspects of the lesions stain with rose bengal.2 Lissamine green is excellent at being able to discern a condition known as “lid wiper epitheliopathy” and SLK when diagnosing dry eye. Questions remain about the toxicity profiles of many dyes, and one may consider rinsing with saline in certain situations, but it is usually not a concern for fluorescein.1,2 Combined with case history, visualization with fluorescein and magnification makes some diagnoses of ocular conditions more certain, ranging from ruptured globe to dry eye. Future directions for vital dyes show promise in not just visualization of the ocular surface but also determining exact concentrations of molecules such as glucose or lactoferrin.4
Statement of Consent
The patient referred to in this video article has given their informed consent to be filmed and is aware that information and images will be published online.
Note
Animation added post-publication on 06/24/2025. No changes were made to the article content.
Citations
- Badaro E, Novais EA, Penha FM, Maia M, Farah ME, Rodrigues EB. Vital dyes in ophthalmology: a chemical perspective. Curr Eye Res. 2014 Jul;39(7):649-58. doi:10.3109/02713683.2013.865759.
- Dhaliwal RS, Dhaliwal KVS, Singh M, Kakkar A. Stains and dyes in ophthalmology. Glob J Cataract Surg Res Ophthalmol. 2022;1:81-7. doi:10.25259/GJCSRO_5_2022.
- In: Reilly J, Gaiser H, Young B. eds. Clinical Procedures for Ocular Examination, 5th Edition. McGraw Hill; 2024. Chapters 5.7-5.9, and 5.12.
- Shi Y, Hu Y, Jiang N, Yetisen AK. Fluorescence sensing technologies for ophthalmic diagnosis. ACS Sens. 2022 Jun 24;7(6):1615-1633. doi:10.1021/acssensors.2c00313.

