Robotic Thymectomy for Myasthenia Gravis
Abstract
Myasthenia gravis is an autoimmune disease affecting acetylcholine transmission involved in skeletal muscle contraction. The approach to myasthenic patients is complex as optimal treatment involves a multidisciplinary technique of combined medical and surgical therapies. Medical therapy with acetylcholinesterases and immunomodulators can provide symptom relief and eliminate feelings of fatigue and weakness. Surgical thymectomy can help by reducing symptoms, preventing recurrence, and reducing daily medication requirements. Thymectomy was traditionally performed via a transsternal approach, but minimally invasive and robotic techniques have become increasingly common. Here, we present our approach for robotic total thymectomy through a left-sided approach.
Case Overview
Background
Myasthenia gravis is an autoimmune disease affecting the postsynaptic nicotinic acetylcholine receptors that control voluntary skeletal muscle function. This is commonly mediated by anti-acetylcholine receptor (anti-AChR) antibodies. The onset and magnitude of disease can vary significantly but usually involves some degree of progressive weakness of the eyes, extremities, or oropharyngeal/respiratory muscles.1 In conjunction with medical therapy, surgery has become standard of care as post-thymectomy patients are more likely to have an improvement and/or resolution of symptoms with less reliance on medical therapy.2, 3
Focused History of the Patient
The patient is a 23-year-old female who was diagnosed with anti-AChR positive generalized myasthenia gravis several years ago. Her primary complaint was fatigue, facial weakness, and double vision. She was maintained on daily prednisone and pyridostigmine but has had progressively worsening symptoms. She has now required escalating doses of corticosteroids and intravenous immunoglobulin infusions for symptom control. She is otherwise healthy with no pertinent past medical or surgical history. She has no family history of myasthenia gravis or other autoimmune disease.
Physical Examination
Physical exam revealed a healthy-appearing young woman with normal vital signs. She has no sensory deficits, tendon reflexes are all normal, and there is no exertional upper or lower extremity weakness. She has mild ptosis that is elicited when holding upward gaze for approximately one minute.
Imaging
The patient underwent cross-sectional computed tomography of the chest that showed thymic hyperplasia without a dominant thymoma. There was no associated lymphadenopathy or invasion to surrounding structures. A representative image is shown in Figure 1.
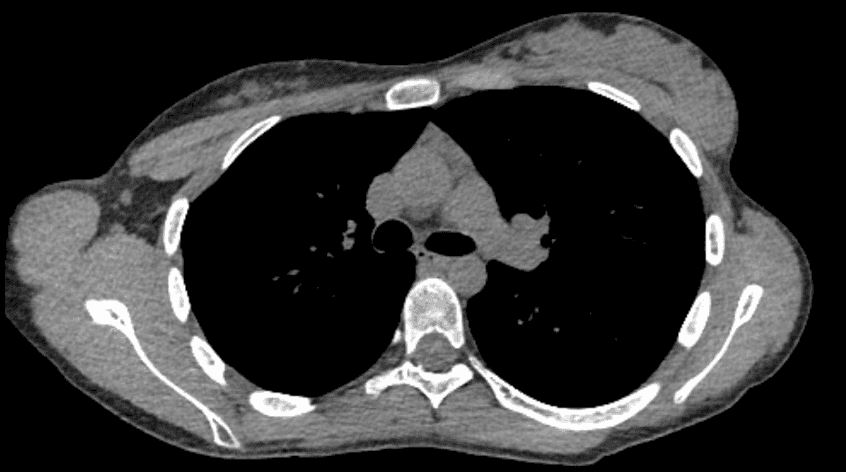 Figure 1. Representative cross-section of axial computer-tomography showing thymic hyperplasia with no dominant thymoma.
Figure 1. Representative cross-section of axial computer-tomography showing thymic hyperplasia with no dominant thymoma.
Options for Treatment
The treatment of myasthenia gravis is typically multidisciplinary and requires cooperation between both neurologists and thoracic surgeons. After diagnosis, patients usually undergo some combination of medical therapy including acetylcholinesterases like pyridostigmine, muscarinics like propantheline, and immunomodulators like corticosteroids, methotrexate, or cyclophosphamide. Infusion of intravenous immunoglobulin (IVIG) may be necessary for refractory disease.1
Once controlled on a stable regimen, most patients are referred for surgical thymectomy, which has been shown to reduce reliance on medical therapies and lessen reported symptoms.
Our video demonstrates a robotic total thymectomy via a left chest approach. Using either thoracoscopic or robotic techniques, minimally invasive thymectomies are increasingly performed using subxiphoid, left, right, or bilateral approaches. Rarely, a transsternal approach may be necessary for large tumors or those with an invasive component.4-6
Rationale for Treatment
Our patient had previously controlled myasthenia that has now required escalating medical therapies. It was thought that thymectomy may allow her to wean from her current medication without recurrence of symptoms.
Special Considerations
Myasthenia gravis patients must be optimized prior to undergoing surgical thymectomy. Following surgery, unoptimized patients may experience “myasthenic crisis”, which presents with profound weakness, respiratory failure, and inability to wean from the ventilator. To avoid this, we planned our intervention one week after her last IVIG infusion and also administered intraoperative stress dose steroids. Additionally, specialized anesthesia techniques including avoidance of paralytics and total intravenous anesthesia were utilized to avoid potential postoperative myasthenic complications.
Discussion
Here we present a robotic total thymectomy via left-sided chest approach. This procedure involves removal of the entirety of the thymus and associated pericardial fat. The borders for this resection include the left and right phrenic nerves laterally, the sternum anteriorly, the pericardium posteriorly, the diaphragm inferiorly, and the superior horns of the thymus superiorly. All fatty tissue within these boundaries is resected while taking care not to injure the important nearby structures including the innominate vein, heart, aorta, and bilateral phrenic nerves.
The patient is positioned supine with a bump under the operative side. This allows full exposure of the left chest while dropping the shoulder out of the field to prevent robotic collisions. Entry is made into the chest at the anterior axillary line in the 4th intercostal space with an 8-mm robotic trocar. Two 8-mm robotic trocars are then placed under direct visualization—one in the midclavicular line in the inframammary fold and another in the posterior axillary line in 3rd intercostal space. Lastly, a 12-mm assistant port is triangulated between the two lower ports in the 5th or 6th intercostal space. Once all the working ports have been placed, the robot is docked. The camera is positioned in the middle robotic port between the two working ports. While there are many options available, our instruments of choice include a Cadiere grasper in the left hand and a long bipolar grasper in the right hand.
Dissection is begun as inferiorly as possible just medial to the phrenic nerve. The fatty tissue of the mediastinum is mobilized off the underlying diaphragm and pericardium in a caudal-to-cephalad fashion. Using a combination of blunt and electrocautery dissection, mobilization continues medially and superiorly until the innominate vein is encountered. This area is approached with meticulous caution and any draining veins to the innominate is controlled with cautery or surgical clips. The right and left superior horns of the thymus are retracted down and dissected free. Lastly, the dissection is carried into the right chest. The right mediastinal pleura can be opened to allow for identification of the right phrenic nerve.
Once the thymus and mediastinal fat is completely mobilized, the specimen is extracted using a retrieval bag from the assistant port. A single Blake drain is used for chest drainage and placed through one of the robotic port incisions. The robot is undocked, and the remainder of the ports are removed and closed with subcuticular sutures.
Postoperatively, the pleural drain was monitored and within normal limits. The Blake drain was removed the following morning and the patient was discharged on postoperative day one. Final pathology was consistent with thymic hyperplasia. On 9 month follow-up, the patient is mostly symptom free except for mild diplopia only present with extreme fatigue. She was weaned to low dose prednisone and no longer requires IVIG infusions.
Author contributions
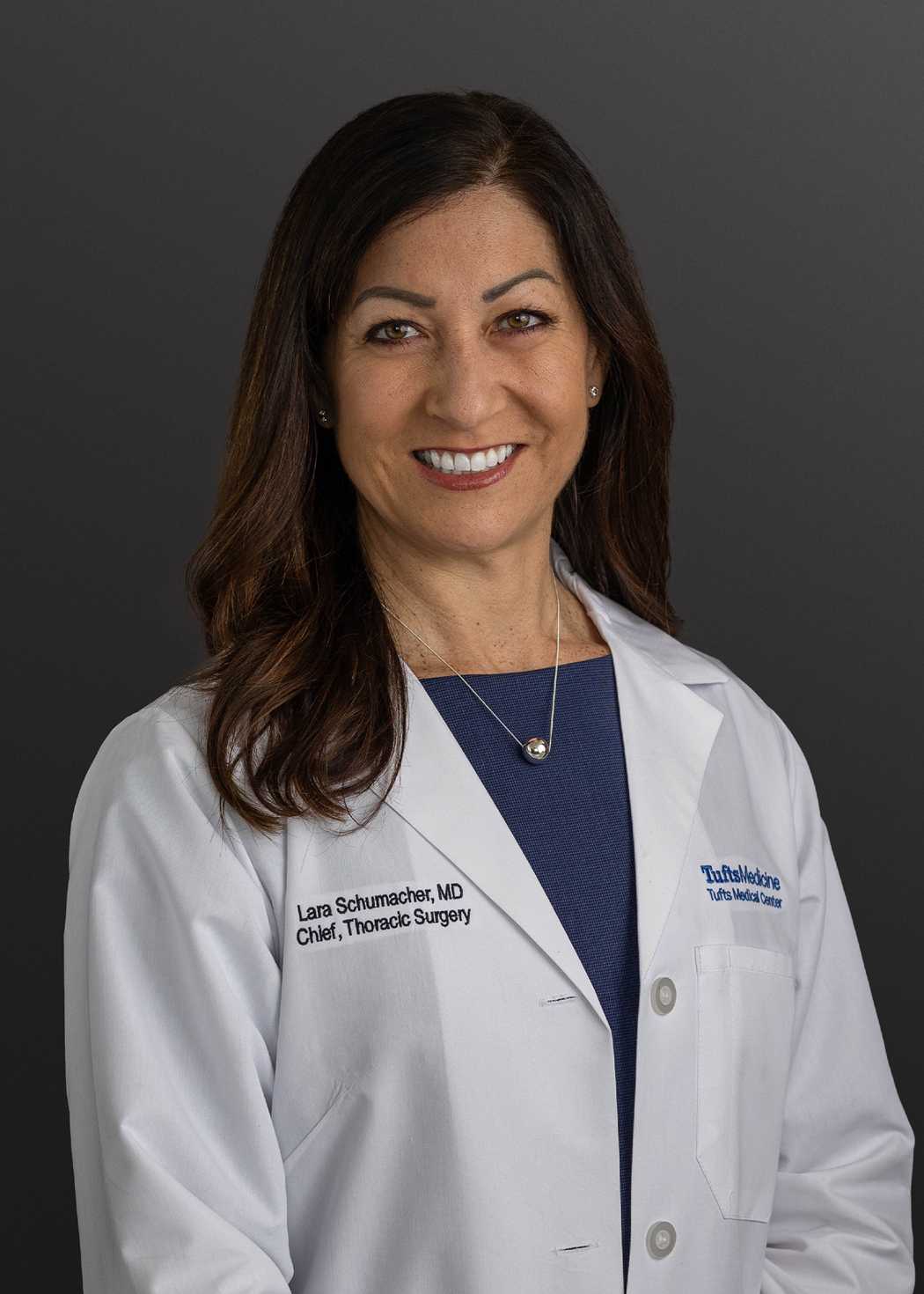
- Constantine Poulos, MD: writing, review, and editing
- Tong-Yan Chen, MD: video production, writing, review, and editing
- Lana Schumacher, MD: video production, writing, review, and editing
Conflicts of interest
All authors declared that there are no conflicts of interest.
Statement of Consent
The patient referred to in this video article has given their informed consent to be filmed and is aware that information and images will be published online.
Note
Animation added post-publication on 10/03/2025. No changes were made to the article content.
Citations
- Vincent A, Palace J, Hilton-Jones D. Myasthenia gravis. Lancet. 2001;357(9274):2122-2128. doi:10.1016/S0140-6736(00)05186-2.
- Gronseth GS, Barohn R, Narayanaswami P. Practice advisory: thymectomy for myasthenia gravis (Practice parameter update): report of the guideline development, dissemination, and implementation subcommittee of the American Academy of Neurology. Neurology. 2020;94(16):705-709. doi:10.1212/WNL.0000000000009294.
- Wolfe GI, Kaminski HJ, Aban IB, et al. Randomized trial of thymectomy in myasthenia gravis. N Engl J Med. 2016;375(6):511-522. doi:10.1056/NEJMoa1602489.
- Marulli G, Comacchio GM, Rea F. Robotic thymectomy. J Vis Surg. 2017;3:68. doi:10.21037/jovs.2017.05.01.
- Wei B, Cerfolio R. Robotic thymectomy. J Vis Surg. 2016;2:136. doi:10.21037/jovs.2016.07.17.
- Holleran TJ, Napolitano MA, Crowder HR, Sparks AD, Antevil JL, Trachiotis GD. Clinical outcomes and technical approach of thymectomy in the veterans health administration. Ann Thorac Surg. 2022;113(5):1648-1655. doi:10.1016/j.athoracsur.2021.05.020.