Transcervical Open Repair of Extracranial Internal Carotid Artery Aneurysm
Abstract
We present the case of a 1.8-cm carotid saccular aneurysm dependent on the left internal carotid, limited to the proximal portion of the bifurcation in a 66-year-old male with a history of hypertension and diabetes mellitus, successfully managed with an open surgical technique. Extracranial aneurysms of the carotid artery are rare and may be caused by atherosclerosis, trauma, infection, or other factors. These aneurysms are characterized by an increase in the diameter of the carotid artery and may require treatment to prevent complications such as embolism or rupture. Treatment may include open surgery or endovascular techniques, and the choice of treatment depends on several factors, such as the location and size of the aneurysm. Medical management may also be considered in selected cases. Diagnosis is made through imaging tests such as duplex ultrasound, computed tomography, or magnetic resonance imaging. It is important to perform a careful evaluation to determine the best treatment option and prevent complications.
Keywords
Carotid aneurysm; carotid disease; arterial hypertension.
Case Overview
Background
Arterial aneurysm is defined as an artery that has at least a 50% increase in diameter compared to the expected normal diameter of the artery. Carotid artery aneurysm may occur as a result of hypertension, atherosclerosis, trauma, dissection, local infection, or after carotid endarterectomy.
Some systematic reviews from 1900 to 2014 reported 1239 patients with 1322 ECAAs.1
The incidence of various etiologies mainly depends on patients' referral and selection. However, over recent years there has been an increase in the incidence of degenerative aneurysms of up to 50–60% and a decrease in the incidence of infectious etiology.2
The true incidence is unknown, but repair represents only 0.6–3.8% of procedures performed for extracranial cerebrovascular disease and is probably <2% of all carotid disease.3,4 For this reason, we report this case to contribute to the knowledge of the incidence of this pathology.
Focused History of the Patient
A case of a 66-year-old male with a history of recently diagnosed arterial hypertension, Stage II, without established treatment as well as recently diagnosed Type 2 Diabetes Mellitus without established treatment is presented. No history of smoking. No allergies, no previous surgeries. Sent for a reference consultation with angiology due to a pulsatile mass in the left neck of 1 year of evolution without pain or focalization data.
Physical Exam
The patient presents an increase in volume in the lateral region of the left neck, pulsating mass. Not painful on palpation, not compressible with G3 left carotid pulse. Without presenting targeting data. Therefore, it is protocolized with an imaging study.
The symptoms of carotid aneurysms vary depending on their location, size, and etiology. The most common finding is a painless pulsating cervical mass, which was the initial symptom in 93% of patients. Aneurysms arising at or proximal to the carotid bifurcation are easily palpable and generally do not present any diagnostic difficulty. Those arising from the internal carotid artery near the base of the skull can cause diagnostic problems. A chronic unilateral swelling of the posterior pharynx should raise the level of suspicion, especially when other physical, strange, or atypical signs are absent.5
Imaging
The patient's angiotomography presents the following finding: left internal carotid artery with a saccular-type aneurysm measuring 1.8 cm in its largest diameter as well as limited to the proximal portion of the bifurcation before the surgery. Patient tomography imaging can be seen in Figure 1.
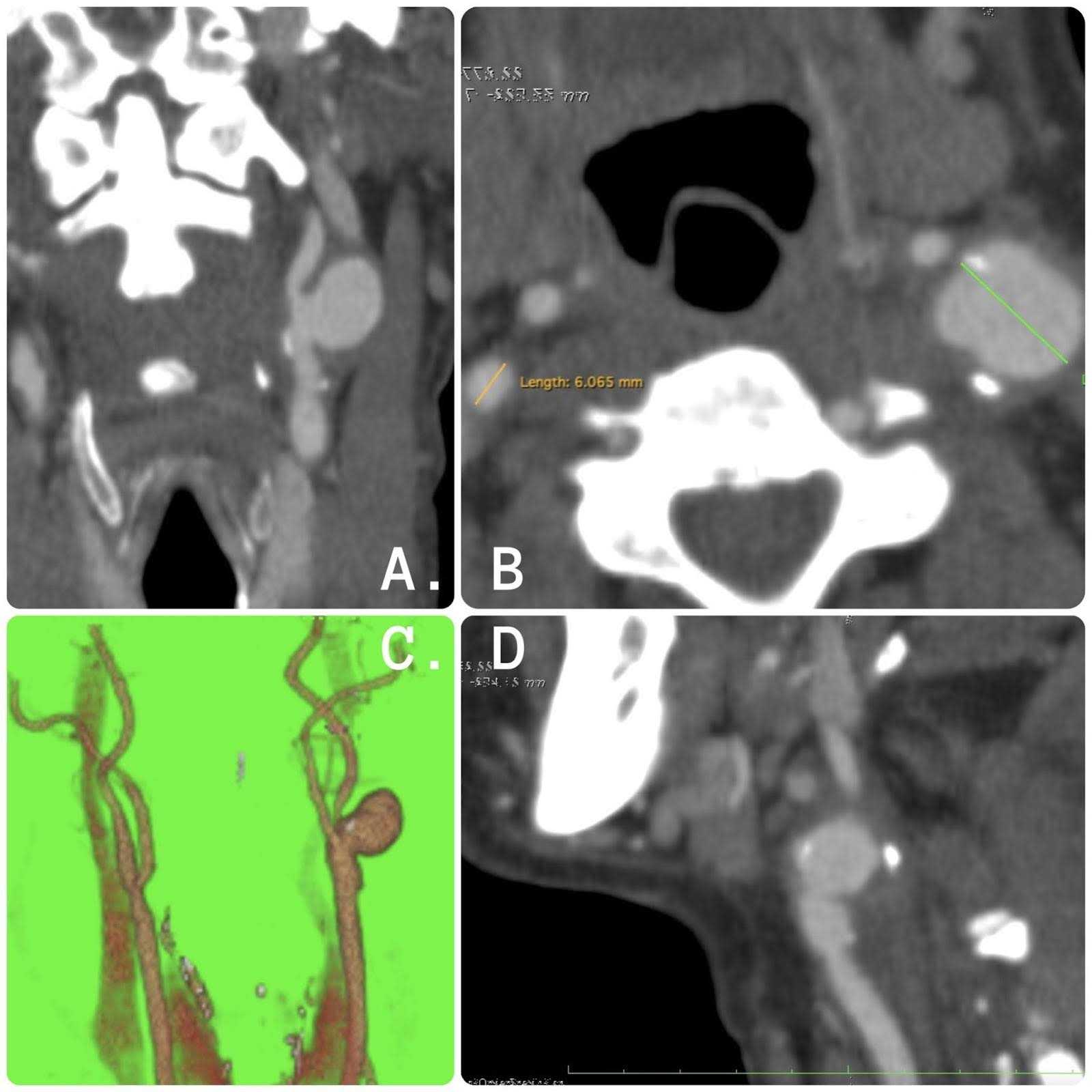
Figure 1. Tomography images. (A) Coronal section with evidence of left internal carotid artery aneurysm with saccular morphology. (B) Axial section with evidence of left internal carotid artery aneurysm of 1.8 cm in greatest diameter. (C) Three-dimensional reconstruction. (D) Sagittal section with evidence of left internal carotid artery aneurysm with atherosclerotic plaque.
We must remember that in the event of a high index of clinical suspicion, computed tomography angiography (CTA) is a “gold” standard for aneurysm diagnostic and defining of anatomical structures.
Aneurysms located high in the distal internal carotid artery (ICA), such as those associated with blunt cervical carotid dissection, are notoriously missed by ultrasound. Such aneurysms require a high index of suspicion leading to additional imaging with tomography and have the advantage of visualizing bone relationships and anatomical landmarks, which are critical in deciding whether a lesion is considered "surgically inaccessible" and requires endovascular intervention.6-7
Among the options are open and endovascular surgical management; The first successful resection and repair was in 1952 and endovascular repair for the first time for carotid aneurysms in the 1990s, and they continue to play an increasingly important role, completely displacing ligation as the only surgical option.8-9
Within the open surgical option, it is feasible for injuries that affect the common carotid artery and the proximal third of the internal carotid artery. Aneurysms that involve distal portions of the ICA may require additional supplements to obtain exposure and distal control. Major nerve injuries range between 4–20%, including the facial, vagus, spinal accessory, hypoglossal, and glossopharyngeal nerves.10
Endovascular treatment of carotid aneurysms offers the advantages of avoiding difficult dissection and eliminating the need for high cervical exposure, reducing the risk of cranial nerve injuries and other procedure-related complications. Although most cranial nerve dysfunction is temporary, the incidence of these lesions reaches 20% in some series.11
Treatment It is worth specifying that medical therapies are only indicated in special cases, so we opted for open surgical management; given that the aneurysm was Limited to the proximal portion of the bifurcation, suitable for a surgical approach.
The exact indications for surgical management are: aneurysms with a high risk of rupture diameter >2 cm, relief of compressive symptoms, erosion into adjacent structures, infection, thrombus, or expansion and high risk of stroke.
Discussion
In the risk factor of age, atherosclerosis, and hypertension, the data of carotid aneurysm are concomitant with abdominal aneurysm aorta. About a quarter of patients with carotid aneurysms also have abdominal aneurysm aorta. Additional screening was performed by ultrasonography of the abdominal aorta is recommended for men aged 65 years by risk factors.12
We found five different types of carotid aneurysm based on the anatomy of the aneurysm. This classification system can be seen in Figure 2 and has proven useful in the surgical literature to describe morphology as well as the basis for selecting a particular surgical approach. The types are as follows:
- Type I carotid aneurysms are short, isolated aneurysms of the internal carotid artery above the carotid bulb.
- Type II carotid aneurysms are long aneurysms of the internal carotid artery, running from the carotid bulb to Blaisdell's line, which is the line between the mastoid process and the angle of the jaw.
- Type III carotid aneurysms are aneurysms of the proximal internal carotid artery and the carotid bifurcation.
- Type IV carotid aneurysms are extensive aneurysms involving the common carotid artery and the internal carotid artery.
- Type V carotid aneurysms are isolated aneurysms of the common carotid artery.13
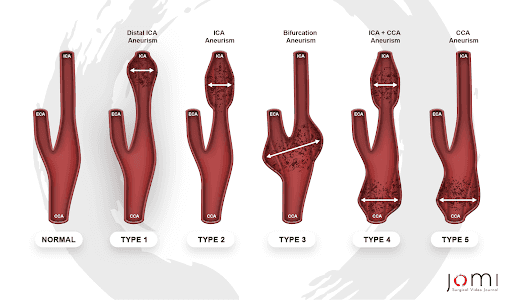
Figure 2. Attigah Classification of Extracranial Carotid Artery Aneurysms.
For this reason, it is essential to carry out surgical planning using the same imaging study that was protocolized in our surgical procedure for type 1 carotid aneurysm based on a conventional carotid endarterectomy approach.
During the operation surrounding fibrotic tissues were dissected, and aneurysm walls were separated and exposed until identified.
Once the aneurysm is identified as well as the structure of the common carotid artery, internal carotid artery, and external carotid artery, external carotid clamping is performed first to avoid prolonged time with internal carotid clamping. The exposure of the surgical field can be seen in Figure 3.
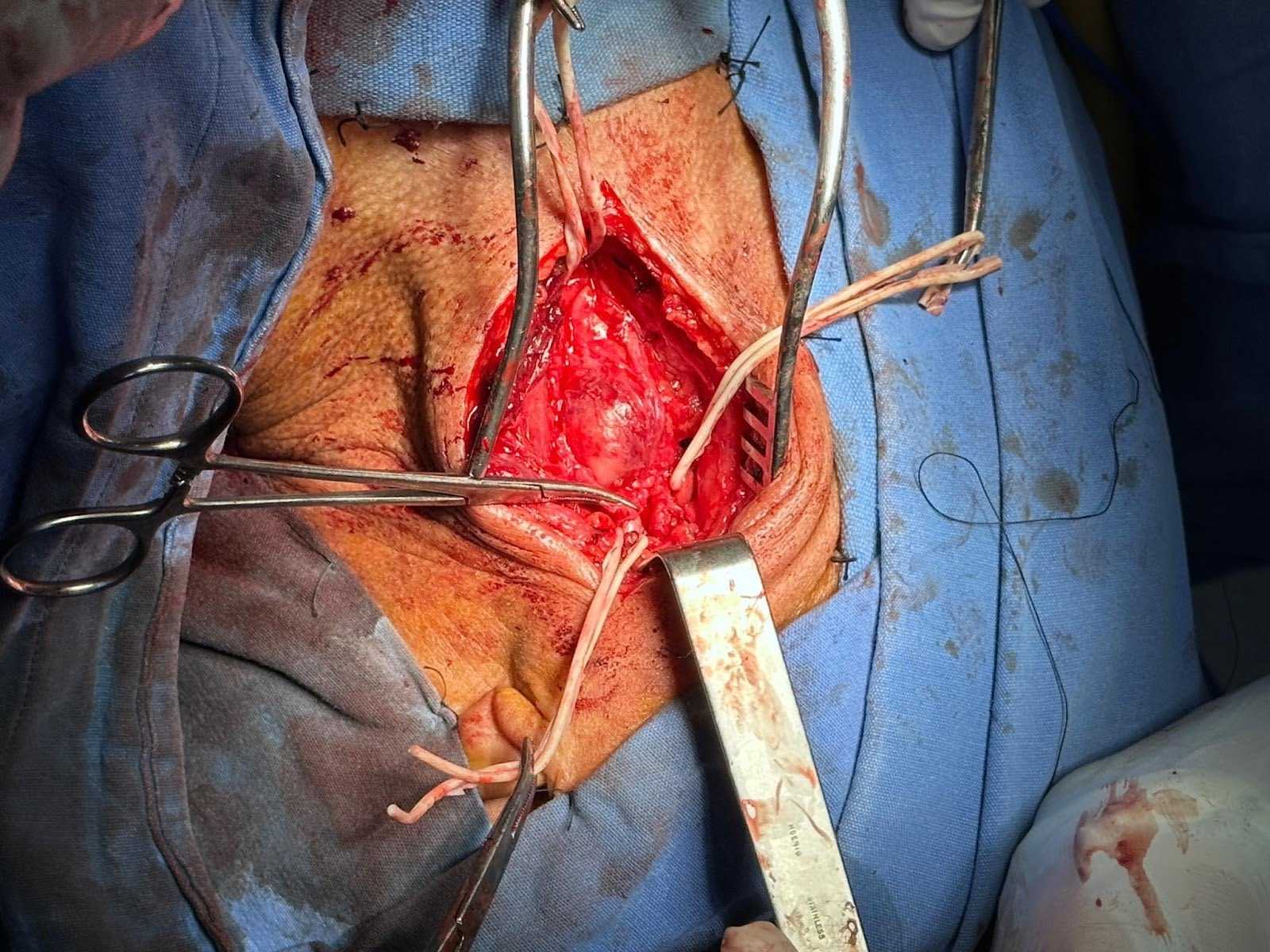
Figure 3. Image of surgical exposure. Reference of common carotid artery, external carotid artery, and internal carotid artery with aneurysm in the proximal portion of the bifurcation.
The external carotid artery is ligated in its distal portion, and the anastomotic mouth is preserved in the proximal portion.
Subsequently, the common and internal carotid artery is clamped from the lower and upper limit of the aneurysm for aneurysmorrhaphy, and the proximal origin of the internal carotid is ligated. Anastomosis was performed with double-armed, non-absorbable monofilament vascular suture using the parachute technique on the proximal external carotid artery and distal internal carotid artery, obtaining aneurysm exclusion and external carotid transposition.
And it shows comparative reconstruction images (Figures 4 and 4) from common carotid artery to internal carotid artery before and after the intervention.
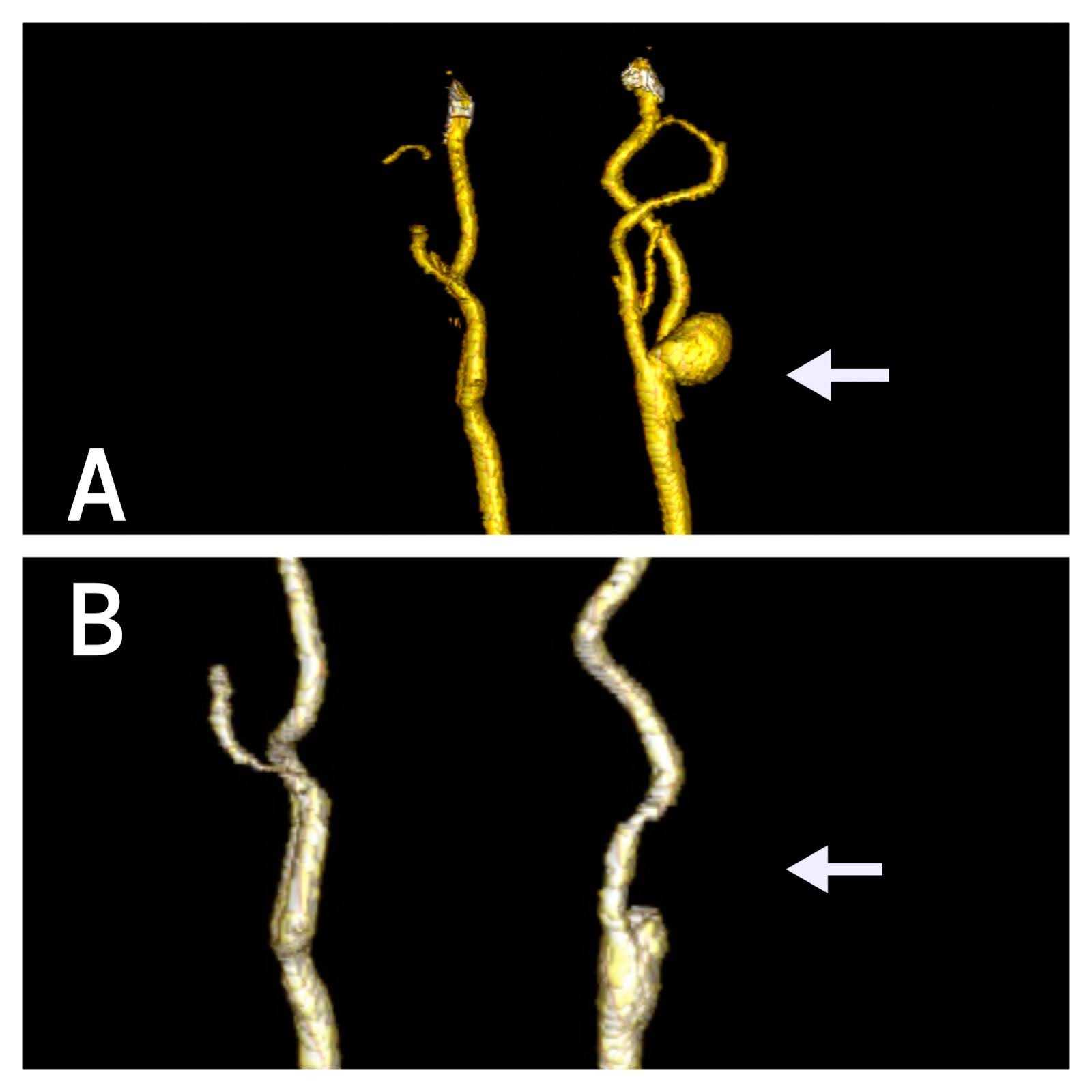
Figure 4. Comparative reconstruction before and after the intervention. (A) 3D comparative (arrow) reconstruction images from common carotid artery to internal carotid artery before surgery. (B) After the intervention.
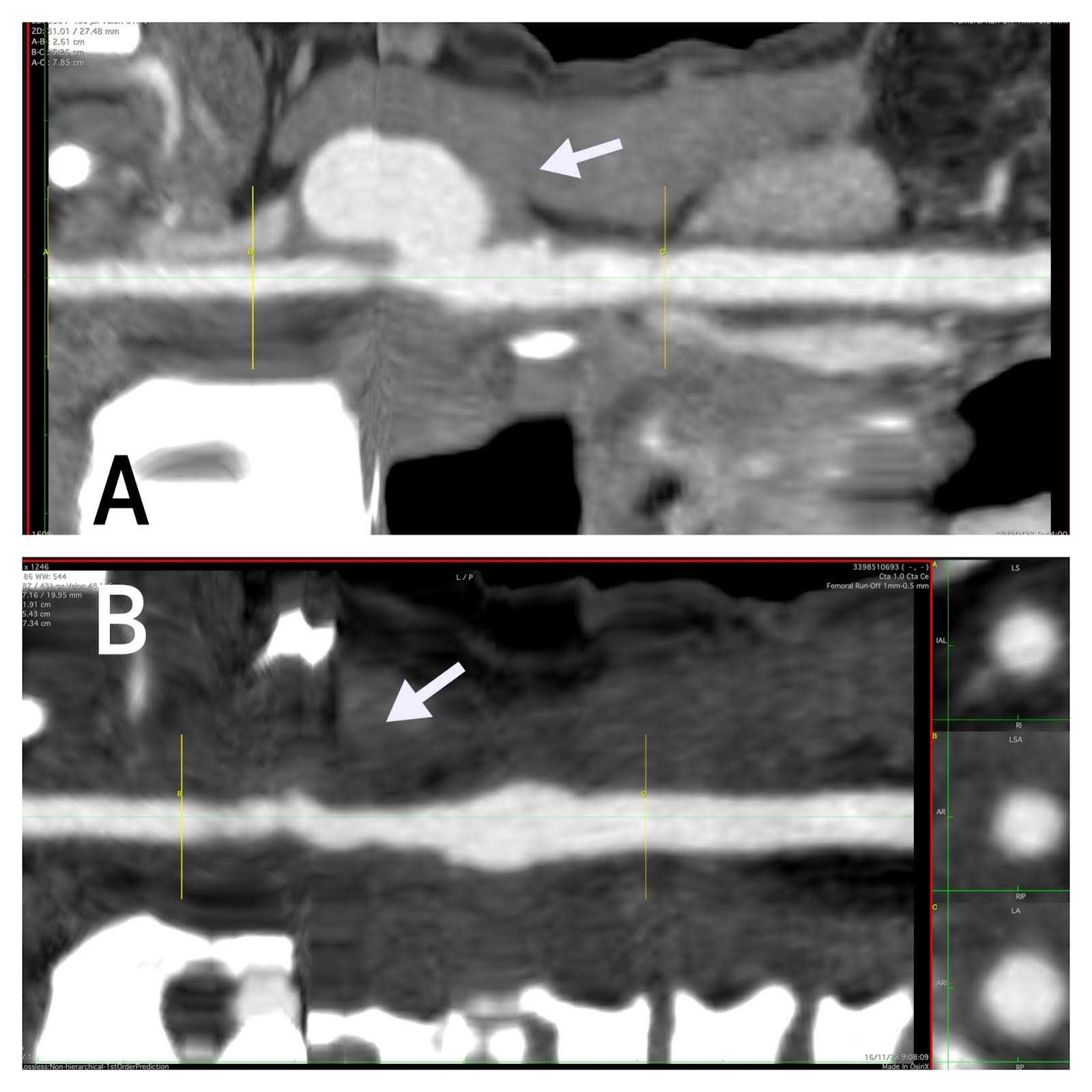
Figure 5. Centerline Comparative. (A) Centerline comparative (arrow) reconstruction images from common carotid artery to internal carotid artery before surgery. (B) After the intervention.
Equipment
For this procedure, it is essential to have a vascular tray, as well as vascular sutures and neurological monitoring always.
Disclosures
Nothing to disclose.
Statement of Consent
The patient referenced in this video article has given informed consent to be filmed and is aware that the information and images will be posted online.
Acknowledgments
A sincere thank you to editor, José Luis Guzmán Colorado, head of imaging for final video editing.
A sincere thank you to Jonathan Monge Duarte and Yarazi Mayan Carrasco Arredondo, translation assistants, and Joel Alonso Rivero Anchondo and Jesus Antonio Loya Silva for image reconstruction, and all the JOMI staff.
Citations
- Welleweerd JC, den Ruijter HM, Nelissen BG, et al. Management of extracranial carotid artery aneurysm. Eur J Vasc Endovasc Surg. 2015;50(2):141-147. doi:10.1016/j.ejvs.2015.05.002.
- Attigah N, Külkens S, Zausig N, Hansmann J, Ringleb P, Hakimi M, et al. Surgical therapy of extracranial carotid artery aneurysms: long-term results over a 24-year period. Eur J Vasc Endovasc Surg. 2009;37(2):127-133. doi:10.1016/j.ejvs.2008.10.020.
- El-Sabrout R, Cooley DA. Extracranial carotid artery aneurysms: Texas Heart Institute experience. J Vasc Surg. 2000;31(4):702-712. doi:10.1067/mva.2000.104101.
- Welleweerd JC, den Ruijter HM, Nelissen BG, Moll FL, de Borst GJ. Management of extracranial carotid artery aneurysm. Eur J Vasc Endovasc Surg. 2015;50(2):141-147. doi:10.1016/j.ejvs.2015.05.002.
- Zhou W, Huang M, Schanzer A, et al. Carotid artery aneurysm: evolution of management over two decades. J Vasc Surg. 2006;43(3):493-496. doi:10.1016/j.jvs.2005.11.023.
- Kato K, Tomura N, Takahashi S, et al. Balloon occlusion test of the internal carotid artery: correlation with stump pressure and 99mTc-HMPAO SPECT. Acta Radiol. 2006;47(10):1073-1078. doi:10.1080/02841850600977745.
- Ritenour A, Bush R. Carotid artery aneurysms. In: Sidawy AN, Perler BA, eds. Rutherford's Vascular Surgery and Endovascular Therapy. 10th ed. Philadelphia, PA Elsevier; 2022:1277-1289. ISBN: 978-0-323-77557-1.
- Pourhassan S, Grotemeyer D, Fokou M, et al. Extracranial carotid arteries aneurysms in children: single-center experiences in 4 patients and review of the literature. J Pediatr Surg. 2007;42(11):1961-1968. doi:10.1016/j.jpedsurg.2007.07.052.
- Saatci I, Cekirge HS, Ozturk MH, et al. Treatment of internal carotid artery aneurysms with a covered stent: experience in 24 patients with mid-term follow-up results. AJNR Am J Neuroradiol. 2004;25(10):1742-1749.
- Berne JD, Dunn E, Rybicki FJ, et al. Sixteen-slice multi-detector computed tomographic angiography improves the accuracy of screening for blunt cerebrovascular injury. J Trauma. 2006;60(6):1204-1209. doi:10.1097/01.ta.0000220435.55791.ce.
- Li Z, Chang G, Yao C, et al. Endovascular stenting of extracranial carotid artery aneurysm: a systematic review. Eur J Vasc Endovasc Surg. 2011;42(4):419-426. doi:10.1016/j.ejvs.2011.05.008.
- Wanhainen A, Verzini F, van Herzele I, et al. European Society for Vascular Surgery (ESVS) 2019 Clinical practice guidelines on the management of abdominal aorto-iliac aneurysm. Eur J Vasc Endovasc Surg. 2019;57(1):8-93. doi:10.1016/j.ejvs.2019.11.026.
- Attigah N, Kulkens S, Zausig N, et al. Surgical therapy of extracranial carotid artery aneurysms: long-term results over a 24-year period. Eur J Vasc Endovasc Surg. 2009;37(2):127-133. doi:10.1016/j.ejvs.2008.10.020.
